Advocacy
Health Disparities
In the United States, the burden of asthma falls disproportionately on Black, Hispanic, and American Indian and Alaska Native populations. Decades of extensive research and public health data identify disparities in asthma prevalence, mortality and health care utilization along racial and ethnic lines.1
Among the more than 27 million people in the U.S. living with asthma, there are serious and persistent racial and ethnic disparities in the burden of illness.2,3 For example:
- Black individuals are about three times as likely to die from asthma than Hispanic or white individuals.4
- Numerous studies show that the prevalence of asthma is greater among Puerto Ricans than any other Hispanic subgroup—or any other racial or ethnic group in the United States.5
- Children with asthma who belong to racial or ethnic minority communities have higher rates of hospitalization, more visits to emergency rooms, and higher mortality rates from asthma than white children.6
- According to an analysis of 2016-2018 data from the Centers for Disease Control and Prevention’s (CDC) National Health Interview Survey (NHIS), 10.4% of American Indian and Alaska Native (AI/AN) individuals have asthma compared to 8.0% of white individuals.7
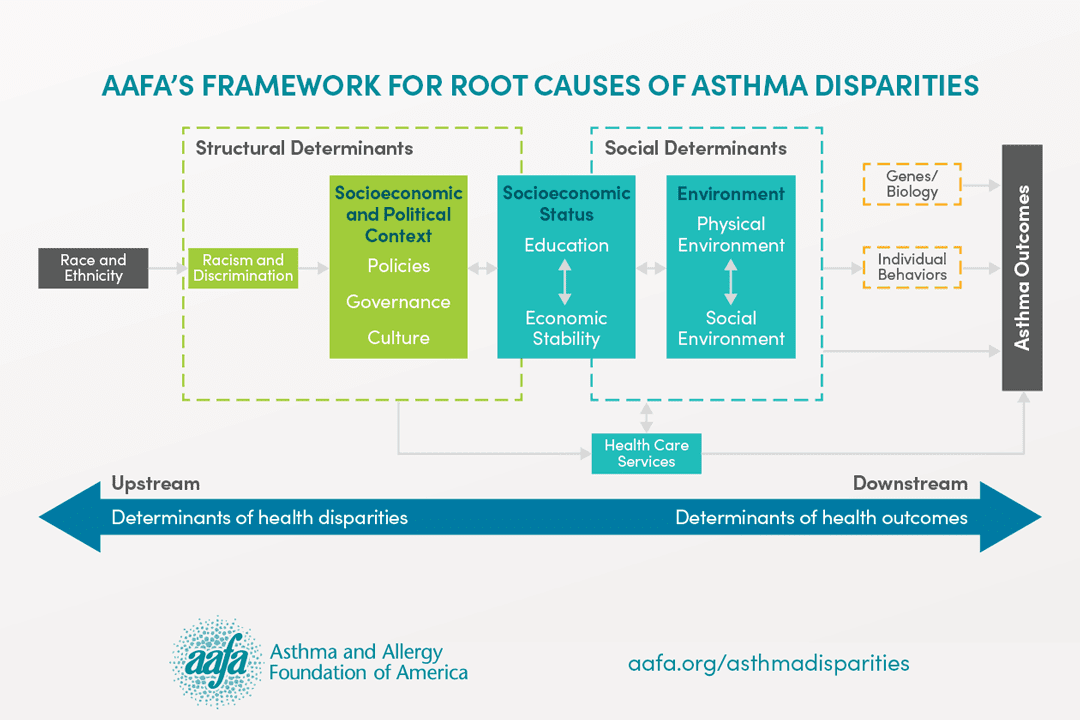
The Asthma and Allergy Foundation of America (AAFA) believes that racial and ethnic disparities are the result of complex interactions among varying levels of social, structural, genetic, and behavioral factors. As noted in AAFA’s 2020 report, Asthma Disparities in America: A Roadmap to Reducing Burden on Racial and Ethnic Minorities, the unequal distribution of stressors, such as poverty, substandard living environments, and lack of access to quality healthcare, can be attributed in part to systemic injustices and racism deeply ingrained in U.S. policies, governance, and culture.8
In 2022, AAFA launched the Health Equity Advancement and Leadership (HEAL) program to address health disparities in communities that bear the heaviest burden of asthma. For more information on HEAL, visit aafa.org/healthequity.
The following principles and strategies should be pursued to achieve equity and help eliminate health disparities for individuals with asthma:
AAFA supports policies that advance equitable access to affordable, quality care and coverage.
Inadequate access to high-quality health care is an important and modifiable contributor to ongoing asthma disparities. Lack of health insurance, limited availability of health care resources, unreliable access to primary and preventive care, unreliable transportation, language barriers, and an inability to take time off work, among others, can all limit access to health care and lead to poor asthma control. Barriers are often magnified by overlapping determinants, such as racism and poverty. Expanding access to high-quality health care that is affordable, comprehensive, and available to all is critical to reducing disparities in asthma.
AAFA supports public policy strategies in the area of health care that:
- Expand health insurance coverage for socioeconomically disadvantaged adults and children
- Improve coverage of asthma guidelines-based care and treatments by expanding specialist care coverage, lowering copays, expanding eligibility criteria, and removing prior authorization and step therapy barriers
- Increase diversity in the primary and specialty health care workforce
- Increase the percentage of minority patients with a “usual source of care” by addressing provider shortage areas, removing financial barriers to office-based primary care services, and expanding the primary care infrastructure to integrate better care coordination
- Develop sustainable models for care coordination and case management that do not place financial burdens on patients
- Encourage and incentivize state and local health departments to adopt comprehensive community asthma programs
AAFA supports policies that create safe and healthy learning environments for all.
Early childhood development and education have significant impacts on the long-term health of a child. Racial and ethnic inequality in education today is rooted in the country’s history of systemic racism and racial segregation. Policies and practices to reduce the racial education gap, increase achievement and opportunities for minority children, and ensure healthy environments in schools have the potential to reduce to health disparities, especially for children with asthma.
AAFA supports public policy strategies in the area of safe and healthy learning environments that:
- Increase access to quality early childhood education and care: Investment in programs like Head Start and Early Head Start will help close the racial education gap by providing access to high-quality early learning, child development, and family engagement for families of young children.
- Create more equitable financial support to schools: Overall, there is a $23 billion funding gap between majority white and majority minority schools. Policies that promote more equitable funding of schools can help address the educational gaps that contribute to poor health outcomes.
- Reduce exposure to environmental triggers by improving school building conditions and improving air quality in and around schools.
- Enact federal and state legislation to put important protections in place for children with asthma and allergies in K-12 schools and child care facilities.
AAFA supports policies that promote safe and healthy physical environments.
Indoor and outdoor physical environments greatly influence an individual’s health and wellbeing, particularly for people with asthma. Exposure to indoor and outdoor allergens and triggers strongly contribute to poor asthma control and exacerbations.
AAFA supports public policy strategies in the area of safe and healthy physical environments that:
- Improve housing quality for rental units, including assisted rental units like public housing, through “healthy home” policies and green building practices.
- Directly finance or support reimbursement models for programs that align asthma clinical interventions with home assessments, indoor environment improvements and remediations to reduce asthma triggers
- Increase access to affordable, quality housing through expanded rental assistance programs, tax credits and inclusionary zoning programs
- Desegregate residential neighborhoods through mobility programs and neighborhood revitalization efforts
- Encourage smoke-free environments
- Combat environmental injustice and reduce exposure to pollution by strengthening clean air policies, reducing transportation-related emissions, restricting zoning of polluting sources and transitioning to a clean energy economy
AAFA supports policies that promote economic stability.
Economic instability is one of the strongest risk factors for asthma. Financial hardship, combined with interrelated factors such as poverty, employment, and income, contributes to socioeconomic disadvantage. Low socioeconomic status has been shown to increase an individual’s exposure to asthma triggers and decrease the ability to seek effective health care.
AAFA supports public policy strategies in the area of economic stability that:
- Increase minimum wage for jobs often held by minority workers
- Reduce the racial wage gap in the U.S. labor market
- Implement tax policies that help low-income families accumulate more wealth
References
- Asthma and Allergy Foundation of America, (2020). [Asthma Disparities in America: A Roadmap to Reducing Burden on Racial and Ethnic Minorities]. Retrieved from aafa.org/asthmadisparities.
- National Center for Health Statistics. (2023). 2022 NHIS Adult Summary Health Statistics. U.S. Department of Health and Human Services. https://data.cdc.gov/d/25m4-6qqq.
- National Center for Health Statistics. (2023). 2022 NHIS Child Summary Health Statistics. U.S. Department of Health and Human Services. https://data.cdc.gov/d/wxz7-ekz9.
- Asthma and Allergy Foundation of America, (2020). [Asthma Disparities in America: A Roadmap to Reducing Burden on Racial and Ethnic Minorities]. Page 40. Retrieved from aafa.org/asthmadisparities.
- Szentpetery, S. E., Forno, E., Canino, G., & Celedón, J. C. (2016). Asthma in Puerto Ricans: Lessons from a high-risk population. Journal of Allergy and Clinical Immunology, 138(6), 1556–1558. https://doi.org/10.1016/j. jaci.2016.08.047
- Anna Volerman, Marshall H. Chin and Valerie G. Press. Solutions for Asthma Disparities. Pediatrics March 2017, 139 (3) e20162546; DOI: https://doi.org/10.1542/peds.2016-2546
- CDC, National Center for Health Statistics, National Health Interview Survey (2016-2018)
- Bailey, Z. D., Krieger, N., Agénor, M., Graves, J., Linos, N., & Bassett, M. T. (2017). Structural racism and health inequities in the USA: Evidence and interventions. The Lancet, 389(10077), 1453–1463. https://doi. org/10.1016/s0140-6736(17)30569-x