Asthma
Asthma During Pregnancy
People with asthma may worry about how their disease may affect their pregnancy and their baby’s health. Asthma may get worse, stay the same, or improve during pregnancy. It is important to control asthma to help you breathe for your baby.
On this page:
Changes in asthma severity
Breathe 4 Baby resources
Does asthma cause complications during pregnancy?
How does uncontrolled asthma affect the fetus?
What should I do to avoid asthma attacks during pregnancy?
Are asthma medicines safe to use during pregnancy?
Are allergy shots safe during pregnancy?
Are flu shots safe to receive during pregnancy?
Can I have asthma attacks during labor?
Is it safe to breastfeed or chestfeed while taking asthma medicines?
Will I pass athma to my baby?
Can I do anything to prevent asthma in my baby?
On this page:
Changes in asthma severity
Breathe 4 Baby resources
Does asthma cause complications during pregnancy?
How does uncontrolled asthma affect the fetus?
What should I do to avoid asthma attacks during pregnancy?
Are asthma medicines safe to use during pregnancy?
Are allergy shots safe during pregnancy?
Are flu shots safe to receive during pregnancy?
Can I have asthma attacks during labor?
Is it safe to breastfeed or chestfeed while taking asthma medicines?
Will I pass athma to my baby?
Can I do anything to prevent asthma in my baby?
Changes in Asthma Severity
For many people, their asthma will remain the same or get better during pregnancy. But, in about 40% (4 out of 10) people, their asthma symptoms will get worse during pregnancy.1
Most people with asthma whose symptoms changed in any way during pregnancy will return to their pre-pregnancy condition within three months after giving birth.
If your asthma symptoms increase or decrease during a pregnancy, you may be likely to experience the same thing in later pregnancies. It is difficult to predict how asthma will change during pregnancy.
Because of this uncertainty, work with your doctors to follow your asthma closely. This way, any change can be promptly matched with an appropriate change in treatment. This calls for good teamwork between you, your obstetrician, your primary care physician, and your asthma specialist.
The Asthma and Allergy Foundation of America (AAFA) with the American Academy of Allergy, Asthma & Immunology (AAAAI) have created Breathe 4 Baby resources. They include tools to help pregnant and lactating people manage asthma during pregnancy and postpartum stages.
Here are other resources for pregnant and lactating people:
- Mother To Baby Resources Webpage – Mother To Baby página web de recursos
- Basics of Asthma and Pregnancy – Conceptos básicos del asma y el embarazo
- Breathing for Two: Managing Asthma During Pregnancy – Respirar por dos: controlar el asma durante el embarazo
- Asthma Medication Fact Sheets – Hojas informativas relacionadas
- Albuterol – Albuterol
- Prednisone – Prednisona/Prednisolona
- Inhaled corticosteroids (ICS) – Corticosteroides inhalados (ICSs)
- Montelukast – Montelukast (Singulair®)
- Salmeterol – Salmeterol (Serevent Diskus®)
- Formoterol – Formoterol (Eformoterol)
- Dupilumab – Dupilumab (Dupixent®)
- Benralizumab – Benralizumab (Fasenra®)
- Mepolizumab – Mepolizumab (Nucala®)
This toolkit was created by the Vaccines and Medications in Pregnancy Surveillance Study Taskforce (VAMPSS), and the Women’s Health in A/I Committee in collaboration with the Asthma and Allergy Foundation of America (AAFA).
The Asthma and Allergy Foundation of America (AAFA) with the American Academy of Allergy, Asthma & Immunology (AAAAI) have created Breathe 4 Baby resources. They include tools to help pregnant and lactating people manage asthma during pregnancy and postpartum stages.
 Pregnancy and Lactation Asthma Action Plan
Pregnancy and Lactation Asthma Action Plan
 Plan de acción contra el asma durante el embarazo y la lactancia
Plan de acción contra el asma durante el embarazo y la lactancia
 Prueba de control del asma durante el embarazo
Prueba de control del asma durante el embarazo
 Conozca las zonas de-asma de su embarazo
Conozca las zonas de-asma de su embarazo
Here are other resources for pregnant and lactating people:
- Mother To Baby Resources Webpage – Mother To Baby página web de recursos
- Basics of Asthma and Pregnancy – Conceptos básicos del asma y el embarazo
- Breathing for Two: Managing Asthma During Pregnancy – Respirar por dos: controlar el asma durante el embarazo
- Asthma Medication Fact Sheets – Hojas informativas relacionadas
- Albuterol – Albuterol
- Prednisone – Prednisona/Prednisolona
- Inhaled corticosteroids (ICS) – Corticosteroides inhalados (ICSs)
- Montelukast – Montelukast (Singulair®)
- Salmeterol – Salmeterol (Serevent Diskus®)
- Formoterol – Formoterol (Eformoterol)
- Dupilumab – Dupilumab (Dupixent®)
- Benralizumab – Benralizumab (Fasenra®)
- Mepolizumab – Mepolizumab (Nucala®)
This toolkit was created by the Vaccines and Medications in Pregnancy Surveillance Study Taskforce (VAMPSS), and the Women’s Health in A/I Committee in collaboration with the Asthma and Allergy Foundation of America (AAFA).
Does Asthma Cause Complications During Pregnancy?
Potential Complications
Asthma is one of the most common medical concerns that occurs during pregnancy. Complications from asthma that is not well-controlled are possible and may include2:
- A small increased risk of preterm (early) labor and delivery
- High blood pressure and a related condition known as pre-eclampsia
- Low birth weight (babies born weighing less than 5 pounds, 8 ounces)
- Low blood sugar in your infant (neonatal hypoglycemia) and seizures
- Birth defects
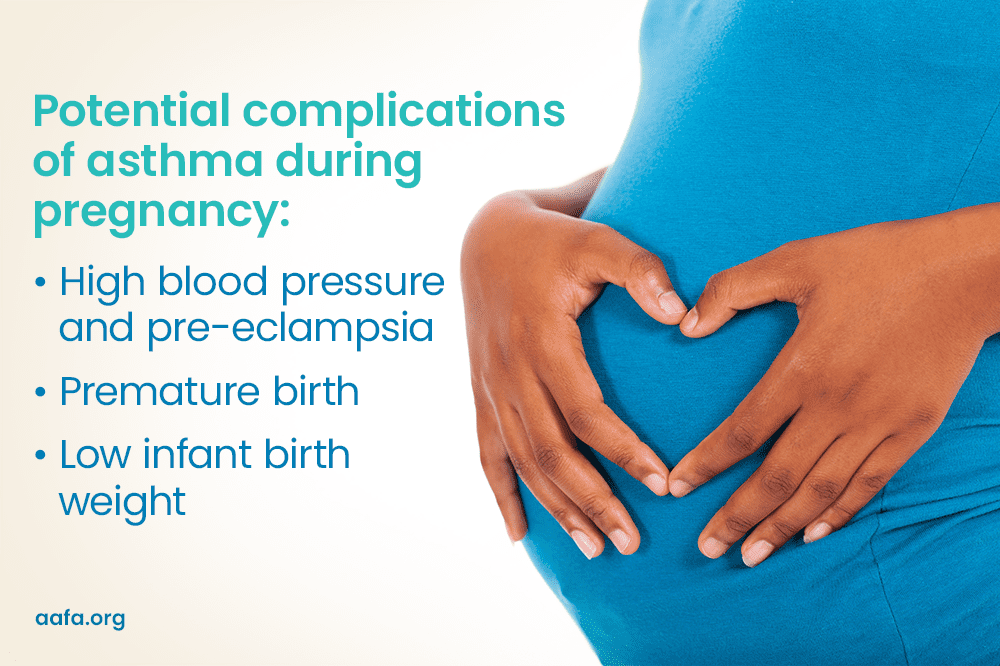
It is not known if asthma is the direct cause of these problems or if other reasons are to blame. Keeping asthma well-controlled may help reduce the chance of complications.
How Does Uncontrolled Asthma Affect the Fetus?
Uncontrolled asthma reduces the oxygen content of your blood. Since the fetus gets its oxygen from your blood, this can lead to decreased oxygen in the fetal blood. The result may impair fetal growth and survival.3 The fetus requires a constant supply of oxygen for normal growth and development.
There is evidence that keeping asthma well-controlled during pregnancy reduces the chances of fetal or newborn death.4 It also improves fetal growth inside the uterus. There are no indications that your asthma contributes to either spontaneous abortion or congenital malformation of the fetus.
What Should I Do to Avoid Asthma Attacks During Pregnancy?
Keep Your Asthma Well-Controlled
Avoiding asthma triggers is always important but is even more important during pregnancy. Take extra steps to avoid asthma triggers to gain the greatest comfort with the least medicine.
- Stay away from people who are sick with respiratory infections.
- Get recommended vaccines (flu, COVID-19, RSV).
- Reduce your exposure to allergens like dust mites, animal dander, pollen, mold, and cockroaches.
- Wear a mask.
- Stay away from tobacco smoke (cigarettes, cigars, e-cigs, vapes).
Stop Smoking Cigarettes/Tobacco
Giving up cigarette smoking is important for any pregnant person. Smoking may worsen asthma and harm the health of the growing fetus as well.
Exercise
Regular exercise is important to health. Talk with your doctor for the best advice about exercising during pregnancy. Swimming is a great exercise for people with asthma. Using quick-relief medicine 10 to 15 minutes before exercise may help you tolerate recommended exercise.
Are Asthma Medicines Safe to Use During Pregnancy?
Is It Safe to Use Asthma Inhalers or Corticosteroids While Pregnant?
During pregnancy, doctors may consider some asthma medicines to be safer than others, so your medicines may change. Work with your doctors to find the best
treatment for you. These include:
- Short-acting inhaled bronchodilators
- Anti-leukotriene agents like montelukast (SINGULAIR®)
- Some inhaled corticosteroids, like budesonide
Note: Montelukast (brand name SINGULAIR®) has a black box warning. This a safety warning from the Food and Drug Administration (FDA). This means you need to be aware of a drug’s side effect or important instructions for safe use of the drug. We encourage you to speak with your health care provider before, during, and after the start of any new medicine. If your doctor recommends montelukast, talk with them about possible risks and concerns.
Long-acting beta agonists (like SEREVENT®, SYMBICORT®, and ADVAIR®) are not considered first-line treatments for asthma in people who are pregnant. But doctors may consider them if your asthma is not well-controlled by the above medicines.
If your asthma is very severe, oral steroids, such as prednisone, may be necessary for the health of you and baby.
Talk with your health care provider to make sure the medicines you are taking are still the right choice. Update your Pregnancy and Lactation Asthma Action Plan as needed.
Remember: It is better for you and your baby if you maintain asthma control (using any approved asthma medicines).
Are Allergy Shots Safe During Pregnancy?
If you are already receiving allergy shots (immunotherapy), you can usually continue if you are not having reactions.
As an extra precaution, though, your allergist may cut the dosage of the allergy extract to reduce the chance of a severe allergic reaction or at a minimum keep the dose the same. But the dose should not be increased during pregnancy since that increases the chance of a reaction.
Are Flu Shots Safe to Receive During Pregnancy?
People with asthma should get flu (influenza) shots. Pregnancy does not change that recommendation. In fact, the flu may be particularly severe in people who are pregnant.
Can I Have Asthma Attacks During Labor?
When asthma is under control, asthma attacks almost never occur during labor and delivery. Also, most people with well-controlled asthma are able to perform breathing techniques during their labor without difficulty.
Is It Safe to Breastfeed or Chestfeed While Taking Asthma Medicines?
Doctors do not believe asthma medicines are harmful to a nursing baby when used in usual amounts. The transfer of asthma medicines into human breast milk has not been fully studied.
When lactating, drinking extra liquids to avoid dehydration is also important (as it is for all people with asthma).
Will I Pass Asthma to My Baby?
Genetics plays a role in whether a baby will develop asthma. In other words, asthma tends to be more likely in a baby if their relatives have it. The environment also plays an important role. For example, babies who are exposed to tobacco smoke or the RSV illness are more likely to develop asthma.
Can I Do Anything to Prevent Asthma in My Baby?
One major prenatal risk factor for the development of asthma is maternal smoking. Giving up cigarette smoking is very important. Other prenatal factors that may influence the development of asthma are:
- Maternal stress
- Diet
- Vitamin D levels
- Antibiotic use
- Method of delivery
Talk with your doctors about identifying your risk factors and making safe changes in preparation for your new baby.
Medical Review: January 2023 by Neeta Ogden, MD; Updated March 2025.
Closed
References
- Bravo-Solarte, D. C., Garcia-Guaqueta, D. P., & Chiarella, S. E. (2023). Asthma in pregnancy. Allergy and Asthma Proceedings, 44(1), 24–34. https://doi.org/10.2500/aap.2023.44.220077
- Shebl, E., & Chakraborty, R. K. (2023, June 26). Asthma In Pregnancy. PubMed; StatPearls Publishing. Retrieved March 14, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK532283/
- American College of Allergy, Asthma & Immunology. (2023, June 28). Pregnancy and Asthma. Retrieved March 14, 2025, from https://acaai.org/asthma/asthma-101/who-gets-asthma/pregnancy-and-asthma/
- Bonham, C. A., Patterson, K. C., & Strek, M. E. (2018). Asthma Outcomes and Management During Pregnancy. Chest, 153(2), 515–527. https://doi.org/10.1016/j.chest.2017.08.029