Asthma Treatment
How Is Asthma Treated?
Although we cannot cure asthma, we can control it. Everyone’s asthma is different, so you and your doctor need to create an asthma treatment plan just for you. This plan will include an Asthma Action Plan that will have information about your asthma triggers and instructions for taking your medicines.
There are three changes in the airways when you have asthma:
- Swelling inside the airways
- Excess mucus that clogs the airways
- Muscles tighten and squeeze around the airways
This swelling, clogging, and muscle tightening makes your airways smaller or narrower. This makes it harder for air to flow easily through your airways, and it becomes harder to breathe. There are asthma medicines that target these three changes. They open your airways and make it easier to breathe.
Learn more about asthma medicines
Use AAFA’s asthma medicine search tool to look up information on specific medicines and their side effects, prescribing information, and possible side effects:
Other resources:
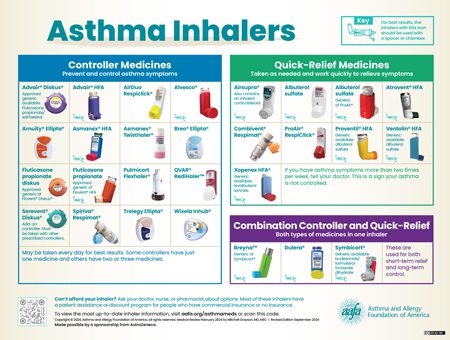
Asthma Inhaler Poster (PDF) (Order Prints)
Asthma Medications During Pregnancy Fact Sheets
What Are the Different Types of Asthma Medicines and Treatments?
There are four types of asthma medicines and treatments:
- Quick-relief medicines – These medicines work quickly to relieve sudden symptoms. You take them as needed and at the first sign of symptoms.
- Controller medicines – These medicines help control asthma by correcting the underlying changes in the airways, such as swelling and excess mucus. They can be one or a combination of medicines.
- Combination of quick-relief and controller medicines – These medicines are used for both short-term relief and control. (They are recommended in the current asthma clinical guidelines, but they have not yet been approved to be used in this way by the FDA.)
- Biologics – This type of treatment targets a cell or protein to prevent swelling inside the airways. They are for people with certain types of persistent asthma and are given by injection or infusion.
The difference between these asthma treatments can be confusing. It is important to understand what each treatment does and how they help your asthma. Learning how to use each correctly can you help keep your asthma well-controlled. Always take your medicines as directed by your doctor and follow your Asthma Action Plan.
What’s the Difference Between Brand Name, Generic, and Authorized Generic Drugs?
Brand name drugs: When a new medicine is created and approved by the Food and Drug Administration (FDA), it is marketed under a brand name. The company that makes it patents the drug. This means this company is the only company that has the right to make and market this drug for a certain number of years, as noted in the patent.
Generic drugs: When a drug patent expires, other companies can make generic versions of the medicine if it follows certain standards set by the FDA. The generic medicines must have the:
- Same active ingredient as the brand name drug
- Same benefits and risks as the brand name drug
- Same strength, dosage, and route of administration as the brand name drug
- Same quality and manufacturing standards as the brand name drug
Generic drugs may be different from brand name drugs in the following ways:
- May be made by the same company or by a different company
- Different look and size, including packaging
- Different inactive ingredients (side effects may vary from the brand name drug because of the inactive ingredients, but this is uncommon)
- Lower costs (most of the time but not always)
Authorized generic drugs: This type of generic medicine is the same as the brand name medicine but without the brand name label. It will have the same active and inactive ingredients as the brand name drug. Authorized generic medicines may also cost less.
If a generic or authorized generic version of a drug exists, health insurance companies may cover those instead of the brand name medicine. Generic drugs can offer the same treatment at a lower cost than brand name.
When it comes to medicines like asthma inhalers and epinephrine devices, the active ingredient and doses will be the same, but the device may look and operate differently. It is very important for you to learn how to use the device prescribed to you even if it is the authorized generic of a brand name device.
What Are the Different Types of Delivery Devices for Asthma Medicines?
You take most asthma medicines by breathing them in using an inhaler or nebulizer. An inhaler or nebulizer allows the medicine to go directly to your lungs. But some asthma medicines are in pill form, infusion form, or injectable form.
Inhalers (also called puffers)
There are four types of asthma inhaler devices that deliver medicine: metered dose inhalers (MDI), dry powder inhalers (DPI), breath actuated inhalers, and soft mist inhalers.
- Metered dose inhalers have medicine plus a propellant. The propellant sprays the medicine out of the inhaler in a short burst.
- Dry powder inhalers do not have a propellant and do not spray the medicine out of the inhaler. The medicine is released from the inhaler when you breathe it in.
- Breath actuated inhalers have a dry powder or aerosol medicine. The medicine does not spray out of the inhaler. The medicine is released from the inhaler when you breathe it in.
- Soft mist inhalers do not have propellant, but they do spray the medicine out of the inhaler. They create a cloud of medicine that sprays out softly.
 For inhalers to work well, you must use them correctly. But 70 to 90% of people who use inhalers make at least one mistake when using their inhaler.1 Inhaler mistakes can lead to uncontrolled asthma. Ask your doctor or nurse to watch you use your inhaler to make sure you are using it correctly.
For inhalers to work well, you must use them correctly. But 70 to 90% of people who use inhalers make at least one mistake when using their inhaler.1 Inhaler mistakes can lead to uncontrolled asthma. Ask your doctor or nurse to watch you use your inhaler to make sure you are using it correctly.
 If you use an MDI, it is best to use a spacer or holding chamber with it. This device attaches to your MDI. It turns the medicine into smaller particles that are easier to inhale.
If you use an MDI, it is best to use a spacer or holding chamber with it. This device attaches to your MDI. It turns the medicine into smaller particles that are easier to inhale.
If an MDI is not easy for you to use, you can also talk with your doctor about a DPI or breath actuated inhaler. These inhalers do not spray medicine out. Instead, you put your mouth around the inhaler’s mouthpiece and breathe in.
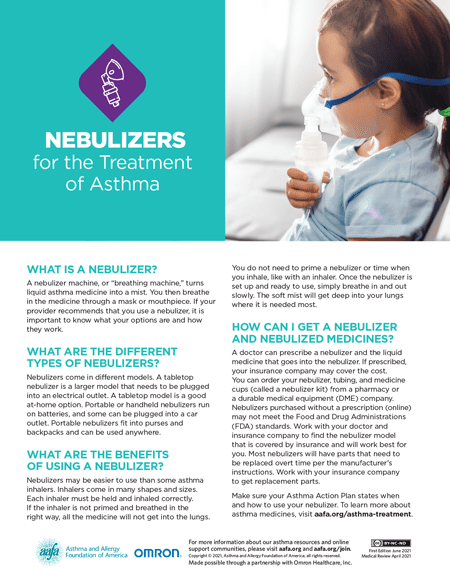
Nebulizers
A nebulizer machine, or “breathing machine,” turns liquid asthma medicine into a mist. You then breathe in the medicine through a mask or mouthpiece.
Nebulizers may be easier to use than asthma inhalers for some people. Once the nebulizer is set up and ready to use, simply breathe in and out as normal.
A doctor should prescribe a nebulizer and the liquid medicine that goes into it. If prescribed, your insurance company may cover the cost. You can also buy a nebulizer from a pharmacy or durable medical equipment (DME) company. Nebulizers purchased online without a prescription may not meet the standards required by the Food and Drug Administration (FDA). Talk with your doctor about which nebulizer is best for you or your child.
Injectables (Biologics)
Injectable asthma treatment (biologics) are shots or infusions given every few weeks. Shots may be given at the doctor’s office or self-administered at home using an auto-injector device, depending on the type of treatment.
Infusions are given intravenously at the doctor’s office. This is when a needle attached to a tube is injected into a vein in your arm. The medicine then drips from a bag, through the tube, and into your arm so it goes into your bloodstream.
How Do Asthma Treatments Work?
Asthma treatments work in these ways:
- They relax the muscles that tighten around the airways. They “relieve the squeeze.” They can be short- or long-acting. By opening the airways, they help remove and reduce mucus. These medicines are bronchodilators [brahn-ko-DIE-ah-lay-tor] or beta agonists.
- They reduce the swelling and mucus inside the airways. These medicines are anti-inflammatories (steroidal and non-steroidal).
Bronchodilators
Bronchodilators can be short- or long-acting. If you use short-acting bronchodilators (quick-relief medicines) more than two days a week, talk with your doctor about your asthma control. You may need to make changes to your treatment plan to better control your asthma.
- Short-acting beta agonists (SABA) are quick-relief medicines. They act quickly and should be taken at the first sign of symptoms. They keep the airways open for four to six hours.
- Short-acting muscarinic antagonists (SAMA) are quick-relief medicines that can be taken with a short-acting beta agonist. They act quickly and should be taken at the first sign of symptoms. They keep the airways open for four to six hours.
- Long-acting beta agonists (LABA) are controller medicines. They are not available as a single medicine. They are found in combination medicines that also have an inhaled corticosteroid. They keep the airways open for up to 12 hours. Only one LABA – formoterol – also acts quickly.
- Long-acting muscarinic antagonists (LAMA) are controller medicines. They are also called anticholinergics and can keep the airways open for 12 to 24 hours. They should be taken daily and will not relieve sudden symptoms.
- Theophylline is a controller medicine that comes as a tablet, capsule, solution, and syrup to take by mouth. It should be taken daily and will not relieve sudden symptoms.
Anti-Inflammatories (Steroidal)
Anti-inflammatories (steroidal) come in many different forms. They are also called controllers because they help to control or prevent asthma symptoms. They reduce swelling and extra mucus inside the airways. They will not relieve sudden symptoms.
- Inhaled corticosteroids (ICS) are corticosteroids that supplement the natural corticosteroids made by your adrenal glands. They are also called controllers because they help to control or prevent asthma symptoms. They target the airways specifically. They can be taken two ways – daily or as needed. If you are taking ICS as needed, take it with your quick-relief medicine – one right after the other. (The FDA has not yet approved these medicines to be used in this way. If you are interested in learning more about this method of treatment, talk with your doctor.) ICS keep working for 12 to 24 hours. Corticosteroids are not the same as anabolic steroids that are taken by some athletes and banned in many athletic events.
- Oral corticosteroids are taken in pill or liquid form. This medicine may be prescribed as “rescue” for the treatment of asthma attacks that don’t respond to other asthma medicines. They also are used as long-term therapy for some people with severe asthma. Oral corticosteroids have serious long-term side effects compared to inhaled corticosteroids. These can include mood swings, weight gain, high blood pressure, cataracts, osteoporosis, and infections.
Other Types of Medicines and Treatments
- Biologics are shots or infusions given every few weeks. They work by targeting a cell or protein in your body to prevent airway swelling. They are for moderate-to-severe asthma that is hard to treat with ICS and/or other medicines, or people with asthma dependent on OCS. They are for specific types of asthma and will not work for everyone.
- Leukotriene modifiers are taken in pill form. They prevent your body from making or activating leukotrienes. The FDA has strengthened existing warnings about serious behavior and mood-related changes with montelukast (Singulair® and generics).
- Cromolyn sodium is nebulized. It is a mast cell stabilizer that prevents the release of certain natural chemicals, such as histamines and leukotrienes into the body.
Single Maintenance and Reliever Therapy (SMART)
The 2020 Focused Updates to the Asthma Management Guidelines recommends single maintenance and reliever therapy, also known as SMART. SMART uses one inhaler that has two medicines (combination medicine) as a quick-relief and controller medicine. When on SMART, you can either take your medicine only as needed to relieve sudden symptoms, or you can take it daily as a controller and as needed for quick relief. This is based on your age and the severity of your asthma.
There is only one long-acting beta agonist – formoterol – that also works as a quick-relief medicine. It acts quickly to open the airways and relieve sudden symptoms. It also works as a controller by keeping the airways open for up to 12 hours. The guidelines recommend using the combination of budesonide and formoterol found in SYMBICORT©. Formoterol is also available with mometasone furoate in Dulera©.
The FDA has not yet approved these medicines to be used in this way. If you are interested in SMART, talk with your doctor.
Will I Always Have to Take the Same Amount of Medicine?
Not always. You will probably take more medicine when you begin treatment to get control of your asthma. Work with your doctor to learn which medicine(s) control your asthma best and how much you need. Once your asthma is well-controlled, your doctor may be able to reduce the amount of medicine you take. The goal is to gain control of your asthma as soon as possible and then control it with as little medicine as possible. Once long-term anti-inflammatory therapy begins, your doctor should monitor you every one to six months. This is to see how your asthma medicines are working and if your asthma is well controlled.
Will I Have to Take Medicine All the Time?
Maybe not. Asthma is a chronic condition (which means you will have it all of your life) that is controllable. Unfortunately, there is no cure for asthma. For that reason, you may have asthma symptoms when exposed to triggers. This is the case even if you don’t have symptoms very often. Your triggers can change over time, and your treatment will depend on two things: how severe your asthma is, and how often you have symptoms. If your asthma is controlled, your treatment will focus on managing symptoms and treatment of episodes when they happen.
If your symptoms happen at certain times and you know what caused them, you and your doctor can use this information to determine the best treatment. If, for example, you have seasonal asthma because of a specific pollen allergy, you may take medicines only when that pollen is in the air. But asthma that specific is not common. Many people with asthma take some form of medicine most or all of the time.
Will Medicine Help Me Sleep Better?
Yes, if you have nighttime asthma symptoms. Many people wake up with asthma symptoms such as coughing or wheezing. You can control nighttime symptoms by taking asthma medicines as directed by your doctor.
Removing triggers where you sleep may help you sleep better. Many people are allergic to dust mites and mold found in bedding materials. Using mattress or pillow encasements can help contain those allergens. Dehumidifiers can also be helpful to reduce the humidity in your home that dust mites and mold need to exist. Using air cleaners in your bedroom may also help reduce your exposure to allergens and irritants (animal dander, dust mites, air pollution, etc.).
Will Medicine Help Me Breathe Better When I Exercise?
Yes. Exercising, particularly in cold air, may cause airway swelling or exercise-induced bronchoconstriction (EIB). Quick-relief asthma medicines, taken before exercise, usually control this. If you need repeated doses of quick-relief medicine during and after exercise talk with your doctor. Your medicines may need to be adjusted. Thanks to these medicines, many Olympic and professional athletes have successful sports careers even with their asthma.
It is important for everyone, including people with asthma, to be as active as possible for good health. Talk with your doctor about how you can be physically active while keeping your asthma well-controlled.
Do Asthma Medicines Have Side Effects?
Yes. All medicines have side effects. Tell your doctor how you are responding to the treatment and if you have any side effects. Follow up often with your doctor so you can control your asthma with the least amount of medicines and with the fewest side effects.
Medical Review: June 2021 by S. Allan Bock, MD; Maureen George, PhD, RN, AEC, FAAN; and Sumita Khatri, MD, MS
References
1. Bonds, R., Asawa, A. and Ghazi, A. (2015). Misuse of medical devices: a persistent problem in self-management of asthma and allergic disease. Annals of Allergy, Asthma & Immunology, 114(1), pp.74-76.e2.