Allergies
Pollen Allergy
Each spring, summer, and fall − and even in the winter in some states − plants release tiny pollen grains to fertilize other plants of the same species. Most of the pollen that causes allergic reactions comes from trees, grasses, and weeds. These plants make small, light, and dry pollen grains that travel by the wind. They then can find their way into your eyes, nose, and lungs, causing allergy symptoms if you have a pollen allergy.
Flowering plants that spread their pollen by insects − like roses and some trees, like cherry and pear trees − do not cause allergic rhinitis.
What Are the Symptoms of Pollen Allergy?
People with pollen allergies only have symptoms when the pollens they are allergic to are in the air. Symptoms include
- Runny nose (also known as rhinorrhea – usually a clear, thin nasal discharge)
- Stuffy nose (due to blockage or nasal congestion)
- Postnasal drip (mucus runs from the back of your nose down your throat)
- Sneezing
- Itchy nose, eyes, ears, and mouth
- Red and watery eyes
- Swelling around the eyes
- Shortness of breath, coughing, and/or wheezing
If you have asthma and pollen makes your asthma worse, you may have allergic asthma. It is the most common type of asthma.
There are 3 main types of pollen allergy: tree pollen allergy, grass pollen allergy, and weed pollen allergy.
Tree Pollen Allergy
Tree pollen is the first pollen to appear each year in the United States. It is responsible for most spring pollen allergy symptoms. It also often overlaps with grass pollen in the spring and summer.
Throughout the U.S., trees produce the most pollen from February through April.1 But in some regions, such as the South, trees may produce pollen as early as December or January and peak at multiple times during the year.
Some of the trees that cause the most allergy symptoms are:
|
|
Grass Pollen Allergy
Grasses cause most late spring and summer pollen allergy symptoms. If you have a grass pollen allergy, where you live may also factor into when you have symptoms.
Grass pollen is most common from April through early June.2 But grass pollen can also be found year-round in warmer parts of the country such as California, Texas, and throughout the South.
There are hundreds of types of grasses, but only a few cause allergy symptoms. Some of the most common types of grasses that cause allergy symptoms are:
- Bahia
- Bermuda
- Fescue
- Johnson
- Kentucky blue
- Orchard
- Rye
- Sweet vernal
- Timothy
Weed Pollen Allergy
Weed pollen, especially ragweed, causes allergy symptoms for many Americans.
Weed pollen appears in the late summer and fall. Ragweed is an invasive annual weed that grows throughout the United States in areas that have been disturbed by human activity. It can travel hundreds of miles in the air. This makes it hard to avoid.
Other weeds are also responsible for weed pollen allergy. Common weeds that can cause symptoms include:
- Burning bush
- Cocklebur
- Lamb’s-quarters
- Mugwort
- Pigweed
- Ragweed
- Russian thistle
- Sagebrush
- Tumbleweed
What Is a Pollen Count?
A pollen count is how much pollen is in the air. To get a pollen count, a device such as an air sampler is used to capture pollen and then the sample pollens are identified and counted. The American Academy of Allergy, Asthma & Immunology’s (AAAAI) National Allergy Bureau™ collects pollen and reports these counts around the U.S.
Some websites or weather news report pollen forecasts also. Pollen forecasts are estimates, just like a weather forecast. Most of the time, pollen forecasts will only report on the most common types of pollen. Pollen counts are more accurate.
This may help you identify which type of pollen is present in your area and triggering your allergy symptoms. Pollen forecasts can help you prepare, but you may feel allergy symptoms at times when the forecast predicted low or moderate amounts of pollen.
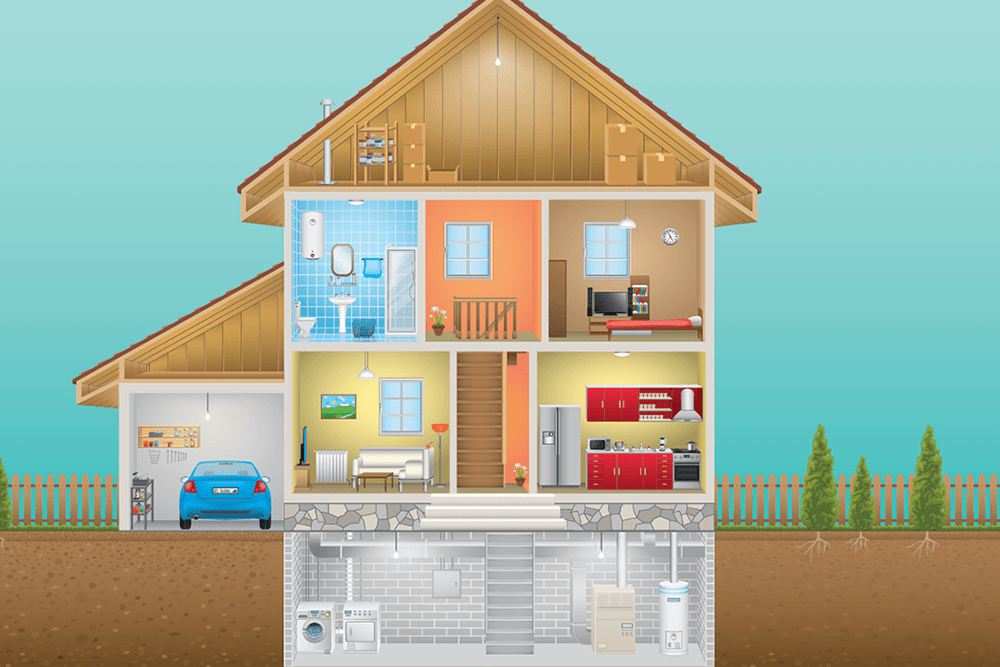
What Is Pollen-Food Allergy Syndrome and How Is It Related to Pollen Allergy?
If you have symptoms of an allergic reaction in your mouth or throat when you eat certain fruits, vegetables, or nuts, it may be related to a pollen allergy. This is called pollen-food allergy syndrome (PFAS), also called oral allergy syndrome (OAS).
PFAS happens because some tree, grass, or weed pollen are similar to the protein in some fruits, vegetables, and nuts.3 Your immune system gets confused and can’t tell the difference between them. Eating these foods may cause your mouth, lips, tongue, and throat to itch or swell. These foods may include apples, cherries, pears, and more.
Most people react to fresh fruits and vegetables. But many people can usually eat the fruits and vegetables cooked or without the skin.
Birch and alder tree pollen, as well as ragweed pollen, cause many PFAS food reactions.
If you think you may have PFAS, talk with an allergist.
How Do Doctors Diagnose Pollen Allergy?
Doctors usually use 2 tests to diagnose a pollen allergy.
Skin Testing
In subcutaneous (prick/scratch) testing, a nurse or doctor uses a device to lightly prick your skin. The device has small drops of each of the possible allergens on each of the applicator tips (usually there are 8 to 10 per device).
If you have the immunoglobulin E (IgE) antibodies (proteins in the immune system) toward that allergen, the spot will turn red, swell, and itch within 15 to 20 minutes. You may also see a wheal. A wheal is a raised, round area that looks like a hive. Usually, the larger the wheal, the more likely you are to be allergic to the allergen.
If subcutaneous testing does not cause a red, swollen reaction, but your doctor believes you are allergic to the pollen, they may do an intradermal test where a small drop of the potential allergen is injected just under the skin. The development of a red, swollen spot in 15 minutes would indicate that you have IgE against that allergen.
A positive skin test to a certain pollen allergen does not necessarily mean you have an allergy. Your doctor will look at the results, your symptoms, and medical history to determine if you have an allergy.
Specific IgE Blood Test
Blood tests are helpful when you have a skin condition or are taking medicines that interfere with skin testing. They may also be used in children who may not do well with skin testing.
Your doctor will take a blood sample and send it to a laboratory. The lab adds the allergen to your blood sample. Then they measure the amount of antibodies your blood produces to attack the allergens. This test is called specific IgE (sIgE) blood testing. (This was previously referred to as RAST or ImmunoCAP testing.)
As with skin testing, a positive blood test to an allergen does not necessarily mean that an allergen caused your symptoms. Your doctor will look at the results, your symptoms, and medical history to determine if you have an allergy.
How Can I Prevent an Allergic Reaction to Pollen?
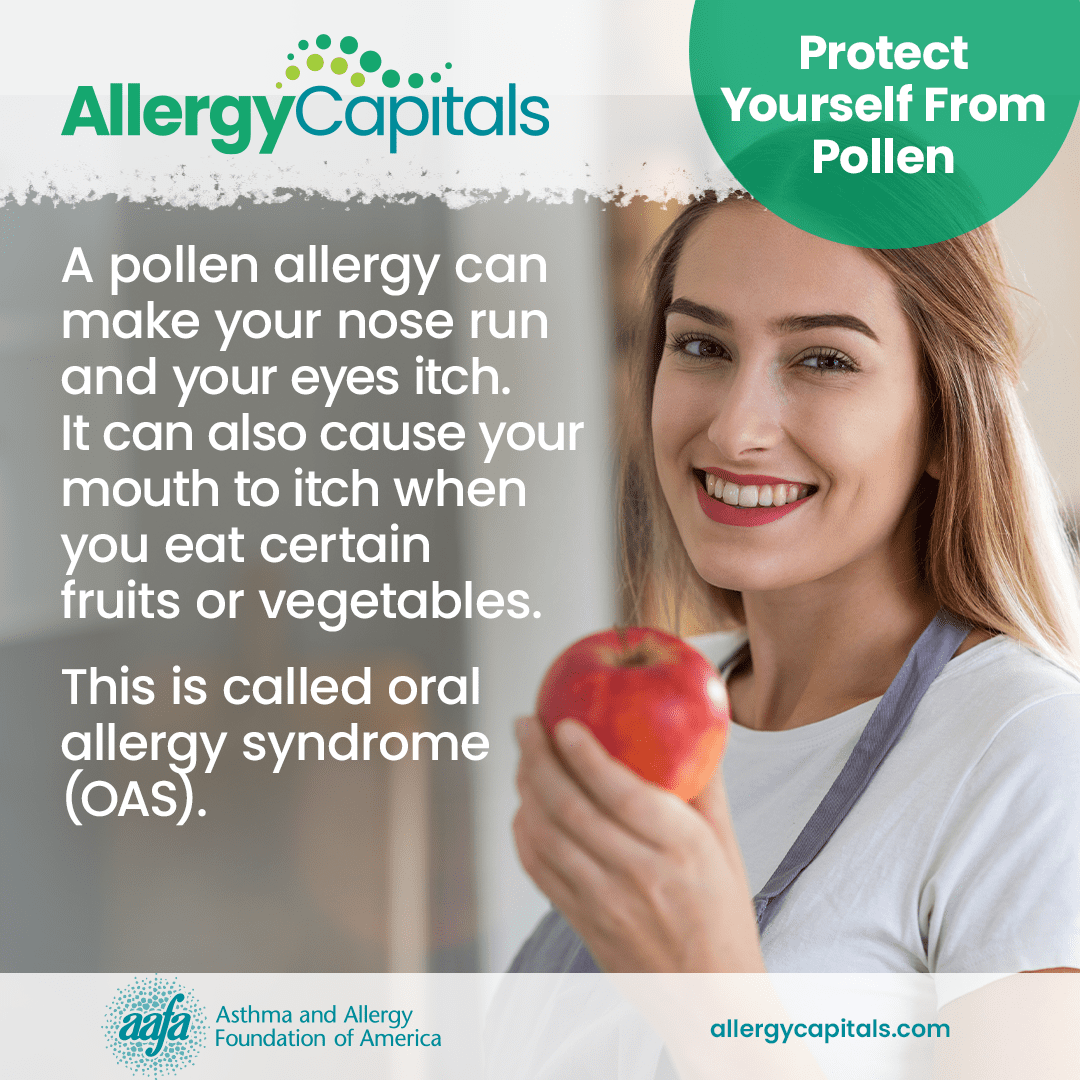
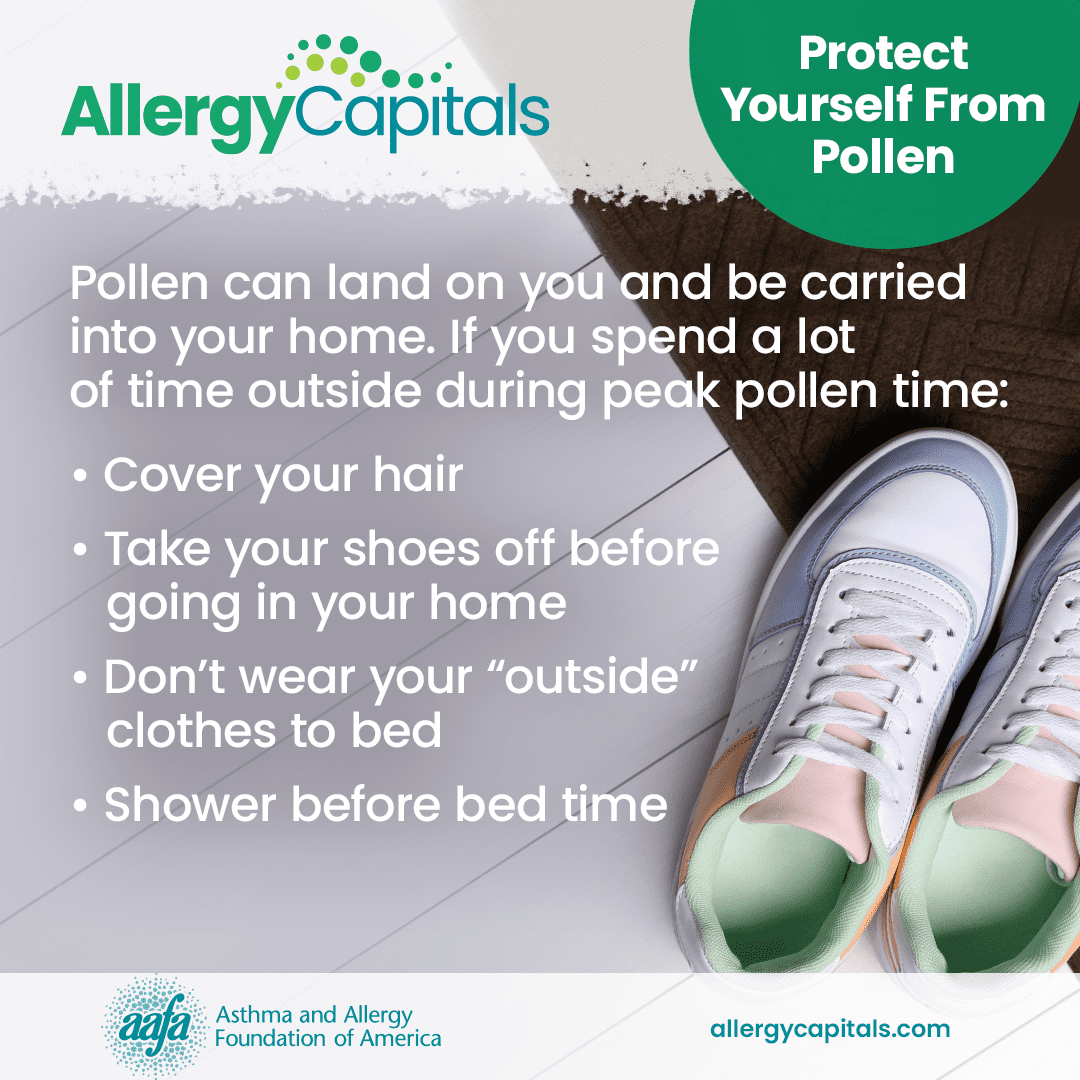
You can help reduce allergic reactions to pollen by reducing your exposure to pollen. This is called environmental control. Here are some actions you can take:
- Start taking allergy treatments before pollen season begins. Most allergy treatments work best when started at least 2 weeks before pollen season begins. This allows the treatments to prevent your body from releasing histamine and other chemicals that cause your symptoms.
- Limit your outdoor activities when pollen counts are high. This will cut down the amount of pollen allergen you inhale and help reduce your symptoms.
- Keep windows closed, if possible, during pollen season or peak pollen times.
- Use central air conditioning or air cleaners with a Certified Asthma & Allergy Friendly® filter and/or HEPA filtration to reduce indoor airborne allergens (including pollen that may enter your home through doors, windows, on your clothes, and on pets), if possible.
- Cover your hair, nose, mouth, and eyes while outside. This will help keep pollen out of your eyes, nose, and airways and off your hair.
- Remove your shoes before entering your home.
- Shower daily before going to bed. This will remove pollen from your body and keep it off your bedding.
- Clean bedding, floors, and fabric furniture once a week.
- Clean blinds, curtains, and washable rugs once a month.
- Limit close contact with pets that spend a lot of time outdoors. Wipe furry animals off when they come inside or bathe them weekly (if appropriate).
- Change and wash clothes worn during outdoor activities.
- Dry your clothes in a clothes dryer or on an indoor rack, not on an outdoor line.
- Watch pollen counts and forecasts. Many local weather reports will give pollen counts or forecasts. You can also visit websites like pollen.aaaai.org for pollen reports.
Allergy Medicine Guide
Nasal rinse: Using a saline (saltwater) nose rinse can help cut down mucus and rinse allergens out of your nose. Remember to use these as directed.
Corticosteroid nasal sprays reduce inflammation (swelling) in the nose and block allergic reactions. They are the most effective medicine type for allergic rhinitis because they can reduce all symptoms, including nasal congestion. They can also provide some relief for eye allergy symptoms. Nasal corticosteroids have few side effects (e.g., headache, nose bleeds or irritation).
Corticosteroid nasal sprays: FLONASE®, Nasacort®, Nasonex™, Nasalide/Flunisolide, Omnaris™, QNASL®, RHINOCORT®
Antihistamines relieve sneezing and itching in the nose and eyes. They also reduce a runny nose and, to a lesser extent, nasal stuffiness. Look for a long-acting, non-drowsy antihistamine. The newer medicines do not carry the risk of toxicity and death that has been associated with older antihistamines like diphenhydramine.
Non-steroidal antihistamine nasal sprays (may cause drowsiness): Astelin®, Astepro®, Patanase®
Non-drowsy oral antihistamines: Allegra®, CLARINEX®, Claritin®
Oral antihistamines that may cause drowsiness in some individuals: Xyzal®, ZYRTEC®
Cetirizine (ZYRTEC®) and loratadine (Claritin®) are the antihistamines of choice for use during pregnancy. They have established safety profiles and are effective in treating allergy symptoms during pregnancy.
Diphenhydramine and related short-acting antihistamines (like promethazine) should be avoided. Diphenhydramine (known under the brand name BENADRYL®) is not a good choice to take for allergy symptoms because of its short-term action to manage symptoms and several known negative side effects. The major side effects of diphenhydramine and older generation antihistamines include drowsiness, sedation, dry mouth/eyes, and fatigue. This can also impair alertness, concentration, multitasking, and memory. In turn, this antihistamine can affect important functions, such as learning and test performance in children, as well as operation of machinery and cars in adults. As these medicines can impair you, they can affect work performance and safety.
Eye drops: Allergy eye drops can relieve eye burning, itchiness, redness, increased tearing, and swelling.
Antihistamine eye drops: Azelastine/Optivar, Bepreve®, Elestat®, LASTACAFT®, Opcon-A®, Systane® ZADITOR®, Patanol™, and Pataday®
Decongestants help shrink the lining of the nasal passages and relieve nasal stuffiness. They generally are only used for a short time (3 days). Read the instructions carefully and do not use them for extended amounts of time. Extended use of decongestant nasal sprays can cause a rebound effect that worsens your congestion. Make sure you talk with your doctor about the appropriate use of decongestants, limitations, and potential side effects.
Nasal spray decongestants: Afrin®, Vicks Sinex™
Oral decongestants: SUDAFED®
Some allergy medicines combine an antihistamine with a decongestant. Certain types of combo medicines (such as the ones that contain pseudoephedrine as the decongestant) are available “behind the counter”. Behind-the-counter products are available without a prescription but have limitations on purchases due to state and federal laws. Talking with pharmacy staff is generally necessary to obtain these types of allergy medications.
Decongestant + antihistamine combos: Allegra-D®, Claritin-D®, Clarinex-D, ZYRTEC-D®
Check with your doctor before using decongestants if you have high blood pressure, heart disease, glaucoma, thyroid disease, or trouble urinating. They may cause issues if you have any of these conditions and they may interact with other prescription medicines.
Federal Regulations on Decongestants
The oral form of phenylephrine (PE) is a common active ingredient in many OTC decongestants. An expert panel of the FDA reviewed studies which showed oral PE is not effective at relieving nasal congestion in commonly used doses. The FDA is proposing to end use of oral PE. This would remove these products from the U.S. market. The change would not affect the nasal spray forms of PE.
Decongestants that contain pseudoephedrine (PSE) require photo identification and are only available to purchase behind the pharmacy counter.
Cromolyn sodium is a nasal spray that blocks your body from releasing chemicals (such as histamine and leukotrienes) that cause allergy symptomsincluding histamine and leukotrienes. This medicine has few side effects, but you must take it three to six times a day. For optimal results, this medication should be used daily during your allergy season. It can be started up to one week before your allergy season begins.
Cromolyn sodium nasal spray: NasalCrom®
Leukotriene receptor antagonists (or modifiers) block the action of important chemical messengers (other than histamine) that are involved in allergic reactions. These medicines help manage asthma and allergic rhinitis symptoms. These medications are taken orally. How often you take them depends on the specific drug. Discuss the appropriate use of these medications with your doctor, including the risks and benefits of therapy.
Options include: ACCOLATE®, SINGULAIR®*, Zyflo CR®
*Note: Montelukast (brand name SINGULAIR®) has a black box warning because it can cause serious mental health side effects. This is a safety warning from the Food and Drug Administration (FDA). This means you need to be aware of a drug’s side effects or important instructions for safe use of the drug. We encourage you to speak with your health care provider before, during, and after the start of any new medicine. If your doctor recommends montelukast, talk with them about possible risks and concerns.
Medical Review: March 2025 by John James, MD
Does Immunotherapy Help Pollen Allergy?
If you have a pollen allergy and do not get complete relief from medicines and environmental control, talk with your doctor about immunotherapy. Immunotherapy is a long-term treatment that can help prevent allergic reactions or make them less severe. It can change the course of allergic disease by changing your body’s immune response to allergens.
There are 2 types of immunotherapy: allergy shots and sublingual immunotherapy.
Allergy shots – subcutaneous immunotherapy (SCIT) has been around for more than 100 years and can provide long-lasting symptom relief. SCIT is a series of shots that have larger amounts of allergen in each shot. The allergen will be injected into the fat under the skin. Over time, allergic symptoms generally improve. Many people get complete relief within 1 to 3 years of starting SCIT. Many people also feel the benefits for at least several years after the shots stop.
Sublingual immunotherapy (SLIT) involves placing a tablet with the allergen under your tongue for 1 to 2 minutes and then swallowing it. In 2014, the FDA approved 3 types of under-the-tongue tablets to treat allergies to grass (GRASTEK®, Oralair®) and ragweed (RAGWITEK®) pollens. You take SLIT tablets daily before and during grass or ragweed season. This treatment offers people with these allergies a potential option instead of allergy shots.
Your doctor may also customize SLIT for you, although this is not approved by the FDA at this time.
Talk with your allergist about your allergy symptoms and your allergy treatment plan.
Closed Accordion
References
1. Lo, F., Bitz, C.M., Battisti, D.S. et al. Pollen calendars and maps of allergenic pollen in North America. Aerobiologia 35, 613–633 (2019). https://doi.org/10.1007/s10453-019-09601-2
2. American Academy of Allergy, Asthma, & Immunology. (2022). Mowing Down Your Grass Allergies. https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/mowing-down-your-grass-allergies
3. Oral Allergy Syndrome Symptoms, Diagnosis & Treatment | AAAAI. (2024, January 10). American Academy of Allergy, Asthma & Immunology. https://www.aaaai.org/Tools-for-the-Public/Conditions-Library/Allergies/Oral-allergy-syndrome-(OAS)
Medical Review: September 2024 by Mitchell Grayson, MD
Allergy Capitals
Your location can have an impact on your seasonal allergies. AAFA’s Allergy Capitals™ report looks at the top 100 most challenging cities in the continental United States to live with seasonal pollen allergies.










 Air Cleaners for Pollen Allergies
Air Cleaners for Pollen Allergies