Allergies
Eczema
Around 16.5 million adults and 8 million children in the U.S. have eczema.1,2 About 60% of people will develop eczema in their first year of life.3 Around 15 to 30% of children and 2 to 10% of adults have eczema at some point during their lifetime.4 Eczema can affect people of all races and ethnicities.
What Is Eczema?
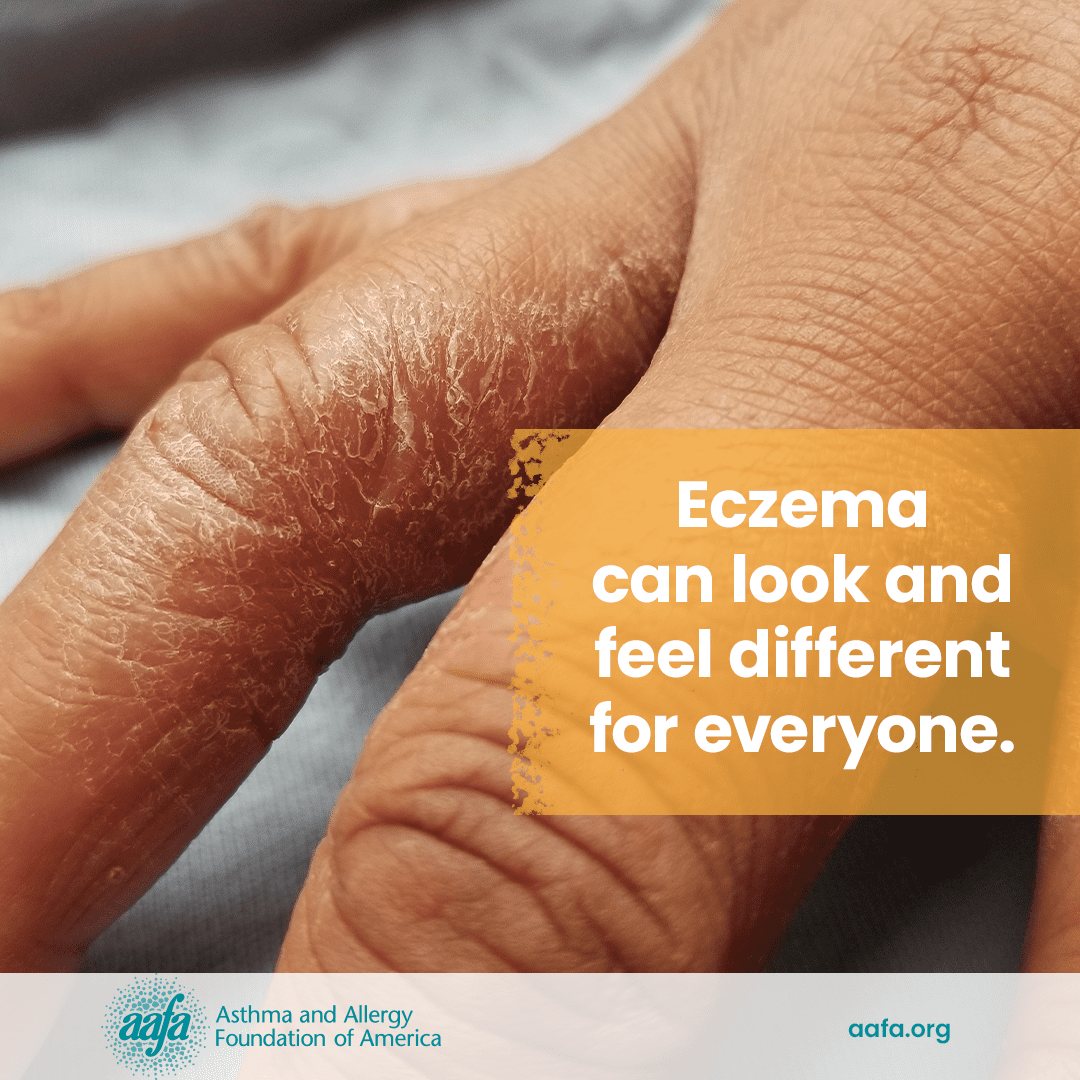
Eczema is a group of chronic skin conditions that cause your skin to become inflamed. It is not contagious. It can cause your skin to be dry, itchy, red, and irritated. You may also develop rashes, blisters, scaly patches, weeping skin, and infections. The affected skin may change color – often gray, purple or deeper brown on darker skin tones and red or pink on lighter skin tones. Over time, the rash may become thick and hard.
Eczema weakens the skin barrier, the barrier that helps your skin hold onto moisture and protects the body from outside irritants, infections, and allergens.

What Are the Different Types of Eczema?
There are several types of eczema. Many are related to allergies.
Atopic dermatitis is the most common form of eczema. Allergens, irritants, chemicals, temperature, and emotions can trigger this type of eczema. Your skin gets dry and itchy, which can lead to rashes and scaly patches. Atopic dermatitis is more common in infants and young children but can occur at any age.
Contact dermatitis is an allergic skin condition caused by irritants and allergies. You usually get a rash soon after an irritant or allergen touches your skin (such as nickel, poison ivy, and latex). This rash is often called allergic contact dermatitis.
Dyshidrotic eczema causes tiny, itchy blisters to appear on your hands or feet. This type of eczema can be painful and result in a burning feeling of the affected skin areas. It can be triggered by an allergy to items such as soaps, nickel, cobalt, sweat, and stress.
Hand eczema is often seen in people who get their hands wet, wash their hands a lot, or are exposed to chemicals often. This can include medical professionals, plumbers, contractors, chefs, and hair stylists. It can cause the skin on your hands to crack and bleed.
Neurodermatitis starts with a patch of itchy skin that becomes itchier as you scratch it. This itch can become intense when you sleep. People with atopic dermatitis, contact dermatitis, obsessive compulsive disorder, and anxiety disorders are more likely to have neurodermatitis.
Nummular eczema causes small, raised, round, itchy spots to appear on your skin. It can be caused by a skin injury like a bug bite or scratch, a skin infection, stress, and heat.
Seborrheic dermatitis is a type of eczema that usually affects your scalp.
Stasis dermatitis occurs in people who have poor blood flow and circulation. It is common on the ankles because poor blood flow usually affects the legs. The affected skin usually becomes discolored.
How Do Doctors Diagnose Eczema?
Primary care providers can diagnose and treat eczema. But they may also refer you to a dermatologist and/or an allergist. They will ask about your medical history, symptoms, and what you think might have caused them. They will also do a physical exam. They may also do tests, such as allergy testing or patch testing. Routine lab work is generally not recommended and can cost a lot.
Physical exam and review of medical history: During your appointment, the doctor will look at your rash and ask when it started and what was happening at that time. Where the rash shows up can depend on your age. Infants usually get rashes on their face, especially their cheeks, and on the outer parts of their arms and legs. Older kids and adults might get rashes in the folds of their arms and legs and sometimes on their hands and eyelids. The doctor might also ask if you did anything or were around something that could have caused the rash.
Allergy test (skin prick or blood IgE tests): Your doctor may test you for allergies through a test on your skin or with a blood sample. For example, it is common for people with atopic dermatitis to be allergic to dust mites.
Patch test: Certain types of dermatitis might suggest contact allergy. If your doctor suspects contact dermatitis, they may ask you to wear skin patches containing small amounts of substances for two days. If you are allergic to the substance, you should develop a local itchy rash. The doctor will do a follow-up exam to check your reaction, usually 2 days after you remove the patch. Common examples of contact allergens include nickel, other metals, cosmetics, latex, and poison ivy.
What Are the Symptoms of Eczema?
Eczema can look and feel different for everyone. It usually shows up on your face, hands, arms, and legs, but it can show up on other parts of the body.
Common symptoms of eczema include:
- Dry skin
- Itchy skin
- Scaly or rough patches on the skin
- Inflamed or swollen skin
- Oozing or crusty skin
- Discolored skin – lighter skin tones may have red patches, while darker skin tones may look ashen white/gray, purple, or dark brown
- Affected skin gets thicker
Children with persistent eczema, late onset, and more severe eczema have frequent or ongoing symptoms. Most children with eczema will outgrow eczema by the time they become an adult.
 |  |
What Triggers Eczema?
Eczema is different for everyone, but knowing what irritates your eczema will help you manage the symptoms.
Common triggers of eczema include:

Allergens (like dust mites, pet dander, certain foods, latex, and pollen)
Soaps, lotions, detergents, and household cleaners
Metals such as nickel (in jewelry, cellphones, belt buckles, etc.)
Stress, emotions, illness, and infections (such as staph skin infections)
Irritants (like fragrances, dyes, chemicals, and formaldehyde)
Changes in temperature (heat, cold, dry weather) and humidity
What Are the Treatments for Eczema?
Managing your eczema involves:
1. Avoiding triggers
Learn what triggers your eczema and do your best to avoid your triggers as much as possible.
2. Over-the-counter and prescription medicines
Treatments are available to help relieve and prevent symptoms for some types of eczema:
- Lotions and barriers to moisturize dry skin and prevent loss of moisture (for example, petroleum jelly, lotions, creams, and ointments)
- Hydrocortisone cream or ointment to reduce inflammation
- Antihistamines to help manage allergies (do not typically help the itching from dry skin)
- Prescription medicines to reduce inflammation, such as:
- Oral or stronger corticosteroid creams and ointments
- Topical calcineurin inhibitors (TCIs)
- Biologics (such as Dupixent® and Adbry®)
- Antibiotics (pills or creams) to treat skin infections
- Phototherapy, the use of ultraviolet light under medical supervision
Treating eczema can help relieve pain and itching, prevent infections, and improve quality of life. Remember to talk with your doctor to help create a treatment and management plan that will work for you.
It’s important to see your doctor regularly to manage your eczema. Your doctor can check your treatment plan and make changes if needed.
3. Appropriate skincare routine
How you treat your skin can affect how well you can control your eczema. Follow these steps to take care of your skin and reduce inflammation and infection.
Bleach Baths
Everyone has bacteria on their skin. The most common is Staphylococcus aureus also known as “staph”. When you have eczema, your skin may get broken open from scratching, and this lets the bacteria get inside the top layers of skin and cause an infection. To help clear up or prevent infections, your doctor may recommend “bleach baths”. This is an option for people with persistent or severe eczema, or who have a skin culture test positive for staph, or when other medical treatments have not worked. Bleach baths decrease the amount of bacteria on the skin. This procedure is safe to do. It involves adding a small amount of bleach to the bath water. It needs to be diluted so that the bleach doesn’t cause irritation.
How to do a bleach bath:
- Fill tub with lukewarm water.
- Add 1/4 cup of bleach to water.
- Soak for 5-10 minutes.
- Repeat 2-3 times per week.
Bleach baths can help reduce the severity of eczema in people prone to skin infections.
Soak and Seal
A key step to taking care of eczema is to help your skin stay moisturized. You can do this by soaking it in water first, then sealing it with a barrier.
- Take short showers or baths (about 5 to 10 minutes) in lukewarm water.
- Don’t scrub your skin and avoid exfoliating products.
- Use a cleanser instead of soap that is unscented and free of perfumes and dyes.
- Pat your skin to dry off. Don’t rub it.
- Use fragrance-free skin products without a lot of preservatives like unscented petroleum jelly, ointments, creams, and lotions. Be sure to use clean hands to apply products.
Wet Wrapping
In people with severe eczema, wet wrapping may be useful. After the soak and seal, you wrap your skin in damp gauze or clothing over the affected areas. This helps the skin stay moist for longer and helps rehydrate the skin.
How to do wet-wrapping for severe eczema:
- Start with the soak and seal method. Do a bleach bath if recommended by your doctor.
- Seal the skin with prescribed skin ointments and creams.
- Wrap the affected skin areas with damp gauze or clothing (e.g. long socks, cotton gloves, leggings, etc.)
- Cover the wet materials with a dry layer of clothing or wraps.
- Sleep with damp gauze over the affected areas of your skin. Warm up your blankets if needed as being wet may make you cold.
Stay Hydrated
Eczema causes moisture loss. Stay hydrated by drinking enough water during the day.
Your doctor can help you create an eczema management plan. Don’t lose hope – there are many treatments that can help manage symptoms and improve your quality of life.
Is Eczema Contagious?
You cannot catch eczema from someone else.
Medical Review: August 2024 by John James, MD
Closed
References
- Eczema in Skin of Color: What You Need to Know. (2018, February 16). National Eczema Association. https://nationaleczema.org/blog/eczema-in-skin-of-color/
- FLG Gene: MedlinePlus Genetics. (n.d.). MedlinePlus. Retrieved September 11, 2024, from https://medlineplus.gov/genetics/gene/flg/#conditions
- Nemeth, V., & Evans, J. (2022, August 8). Eczema. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538209/
- Chiesa Fuxench, Z. C., Block, J. K., Boguniewicz, M., Boyle, J., Fonacier, L., Gelfand, J. M., Grayson, M. H., Margolis, D. J., Mitchell, L., Silverberg, J. I., Schwartz, L., Simpson, E. L., & Ong, P. Y. (2019). Atopic Dermatitis in America Study: A Cross-Sectional Study Examining the Prevalence and Disease Burden of Atopic Dermatitis in the US Adult Population. Journal of Investigative Dermatology, 139(3), 583–590. https://doi.org/10.1016/j.jid.2018.08.028