Asthma
Respiratory Syncytial Virus (RSV)
RSV usually causes mild symptoms. Most people get better in a week or two. But RSV can be serious, especially for infants, older adults, and people who are immunocompromised. Typically, the RSV season in the U.S. starts in the fall and peaks in the winter months, but the timing and severity of the RSV season can vary from year to year.
In children, this infection leads to millions of hospital stays each year, much like the flu. In adults, RSV can cause severe respiratory illness that can make underlying conditions such as chronic obstructive pulmonary disease (COPD) and heart failure worse.2
What Are the Symptoms of RSV?
It can take as long as 4 to 6 days after contact with RSV before someone has symptoms. Symptoms include:
- Runny nose
- Stuffy nose
- Eating less or not interested in eating
- Coughing
- Sneezing
- Red, inflamed eyes (conjunctivitis)
- Fever
- Wheezing (a whistling sound when breathing)
Symptoms in very young infants may be different. They can include:
- Being irritable or cranky (fussiness)
- Eating or drinking less or not interested in eating
- Decreased activity and poor responsiveness
- Trouble breathing (for example, cough, shortness of breath, wheezing, and respiratory distress)
- Faster breathing than usual
- Pauses in breathing that last more than 10 seconds
Call your child’s doctor right away if your child is having trouble breathing, not drinking enough fluids, not responding well, and/or their symptoms are getting worse.
If you or your child have any of the above symptoms, ask your doctor to test for COVID-19, flu, and RSV. It is possible to have any of these illnesses at the same time.
RSV may have symptoms similar to other respiratory illnesses, asthma, and allergies. Our chart below lists the different symptoms for RSV, the flu, COVID-19, the common cold (caused by other viruses), asthma, and seasonal allergies.
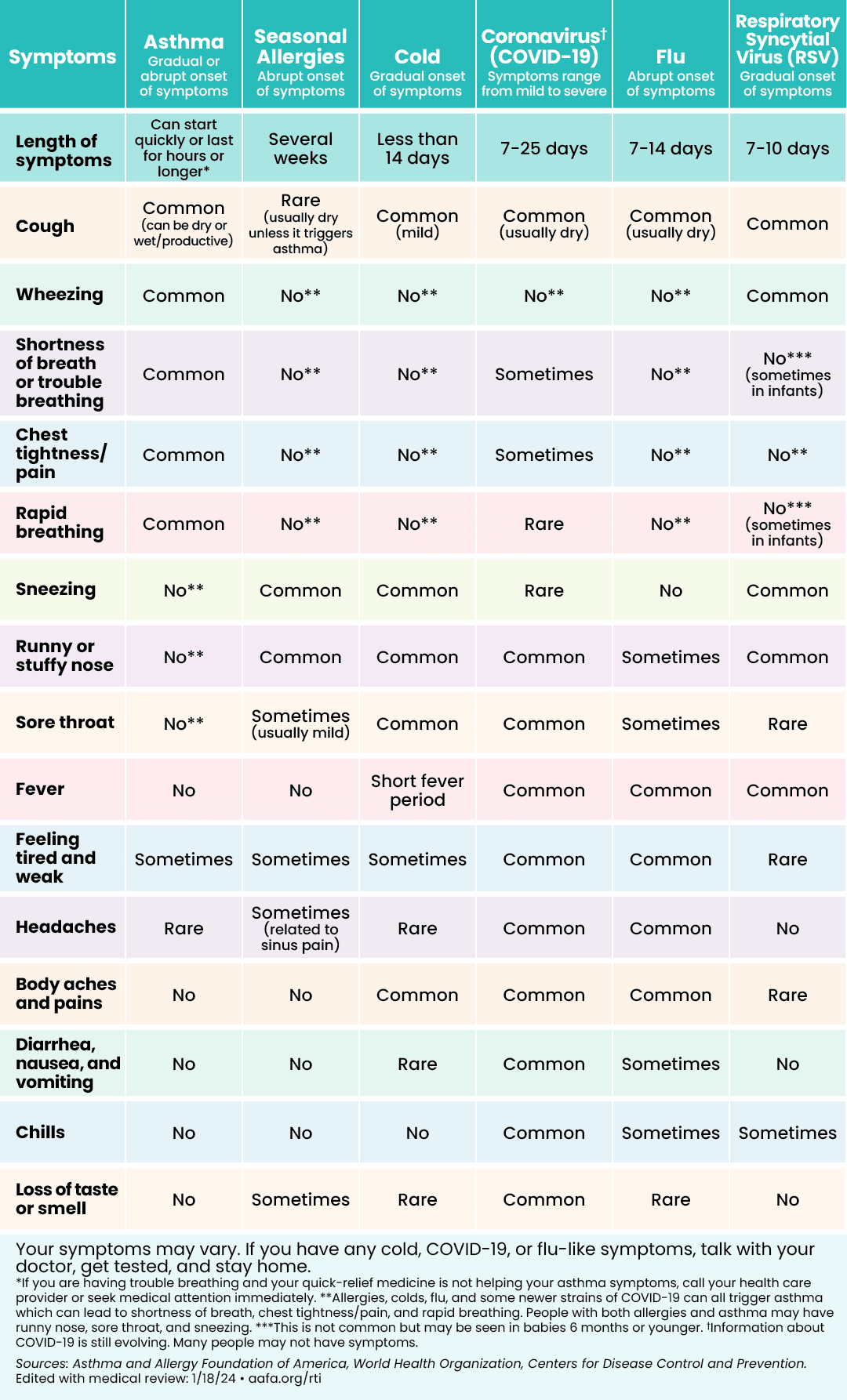 | 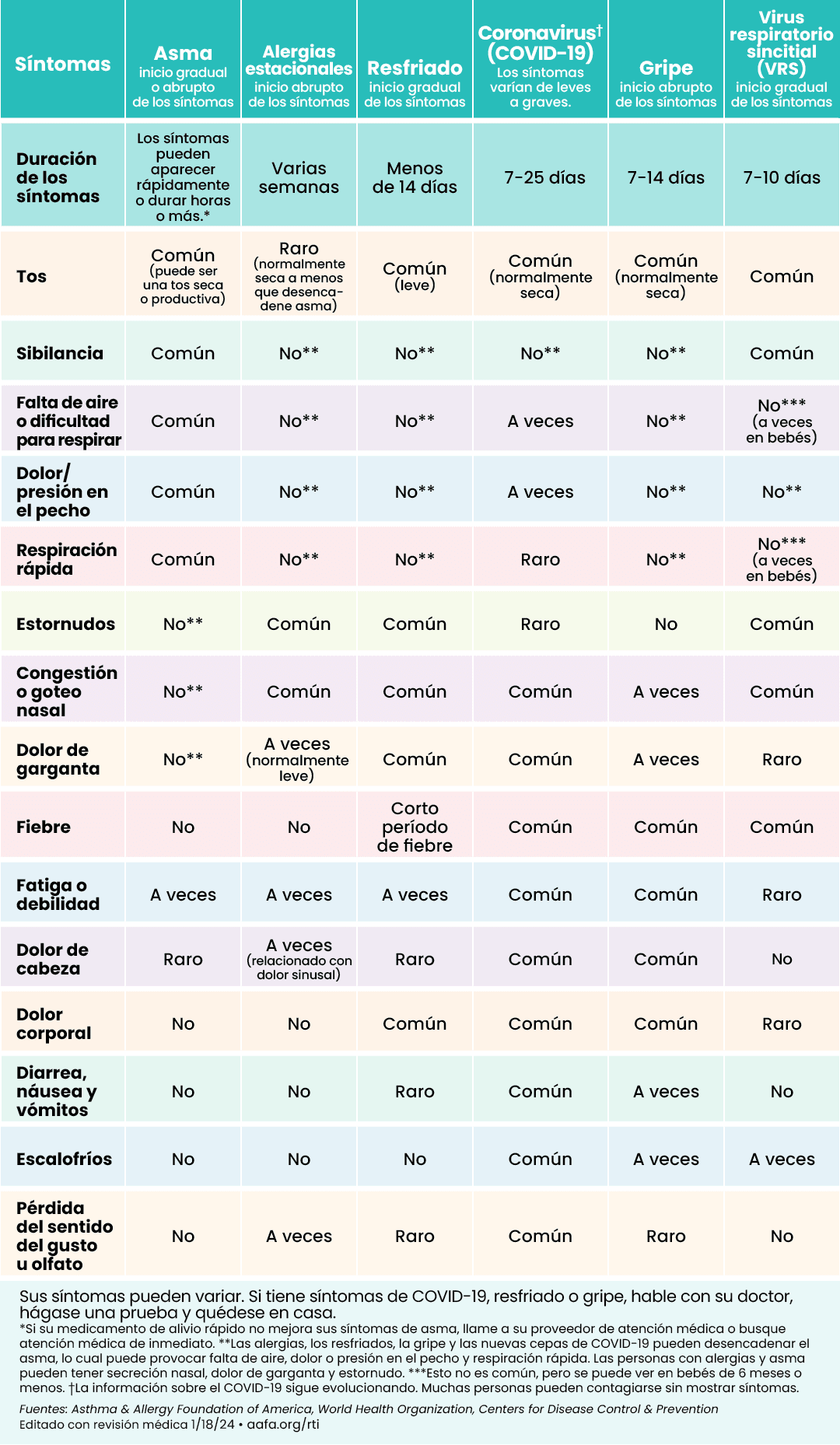 |
Click to see larger image (English) | Click to see larger image (Spanish) |
How Does RSV Spread?
RSV spreads when people talk, laugh, cough, and sneeze. The virus droplets get into the air, and then you breathe them in. The droplets can also land on surfaces, like a doorknob or toys. You can catch the infection by touching the surface with the virus on it and then touching your face. The virus can live on hard surfaces, such as a table or crib rail, for many hours.
You can also get RSV from direct contact, like kissing someone with RSV. Children often come in contact with RSV at day care centers or in schools.
People of any age can get RSV, but it typically affects infants and toddlers. If you have a certain medical condition, the infection may be more severe.
Who Is at High Risk From RSV?
Adults who have the highest risk of severe illness and complications (serious health problems) from RSV infection include:
- Older adults, especially people 75 and older
- Adults with chronic heart or lung disease, such as asthma, COPD, heart failure, cystic fibrosis, or congenital heart disease
- Adults with weakened immune systems or immune deficiencies
- Adults living at high altitudes (8,500 feet or 2,500 meters or higher)
Infants and young children are also at high risk. Children at greatest risk for severe illness from RSV include:
- Premature infants
- Very young infants, especially ages 6 months and younger
- Children younger than 2 years old with chronic lung disease (like asthma or cystic fibrosis) or heart disease (present from birth or congenital heart disease)
- Children with neuromuscular disorders – this includes children who have trouble swallowing or clearing mucus
- Children with Down syndrome
Can RSV Cause or Affect Asthma?
Like the flu, RSV is a lung infection that can trigger asthma. You may not feel or see symptoms of RSV the first 2 days you are sick. By day 3, you may start to feel congested, have a runny nose, fever, or may start to cough, wheeze, and have trouble breathing. People with asthma may have more severe asthma symptoms when they have RSV.
If you or your child have asthma and get sick with RSV, be sure to follow your Asthma Action Plan. Know asthma warning signs and symptoms. Call your health care provider if you or your child have trouble breathing, wheezing, a cough that gets worse, or symptoms that don’t get better or get worse.
There is a link between RSV infection in young children and the chances of developing asthma later in childhood.
RSV is the leading cause of hospital stays in young children and infants. Babies who get sick with RSV are more likely to have asthma later in childhood.3
What Is the Treatment for RSV?
If you have asthma, contact your doctor right away if you have symptoms of RSV. If your infant has RSV symptoms – whether they have asthma or not – contact their doctor.
Most RSV infections will go away on their own in about 7 to 10 days. RSV is caused by a virus, so antibiotics will not help. Talk with your doctor about taking over-the-counter medicines to help with symptoms, like pain relievers or cough and cold medicine. Be sure to talk with your doctor about how to take these medicines appropriately. Ask about nasal suction and lubrication – such as a nasal saline spray, mist, or drops – which may help ease congestion. Drink plenty of fluids and rest. Limit your time around other people to prevent spreading RSV.
Are There Vaccines and Treatments for RSV?
An RSV vaccine is available for infants and babies, pregnant people, and some older adults.
Talk with your doctor about the RSV vaccine if you:
- Are an adult 75 years of age and older
- Are an adult 60 to 74 years and older AND at an increased risk of RSV disease (see risk factors in the section, “Who Is at High Risk from RSV?”)
- Live in a nursing home or long-term care facility
- Are 32 to 36 weeks pregnant during RSV season (usually September through January)
The vaccine can help prevent lower respiratory tract disease that is caused by the RSV virus. It is a one-time dose vaccine and can be given at the same time as other vaccines.
There are also prescription medicines that provide protection against RSV for certain infants and young children, especially against severe illness. They are monoclonal antibody shots. They have proteins that stimulate your child’s immune system to fight RSV.
Nirsevimab (brand name Beyfortus) is recommended for:
- All infants younger than 8 months born during RSV season or entering their first RSV season. (If you got the RSV vaccine while you were pregnant, your infant may not need nirsevimab if they are younger than 8 months and were born 14 or more days after you got RSV vaccine.)
- Some children aged 8 through 19 months who are at increased risk for severe RSV disease and entering their second RSV season:
- Children who have a chronic lung disease because they were born prematurely
- Children who are severely immunocompromised
- Children with cystic fibrosis who have severe illness
- American Indian and Alaskan Native children
Palivizumab (brand name Synagis) is only for certain infants and children under 24 months old who are at high risk. This can include:
- Infants born prematurely (less than 29 weeks)
- Premature infants with chronic lung disease
- People with congenital heart disease (present from birth)
Palivizumab must be given once a month during RSV season. Dosing is based on your infant’s weight. Talk with your doctor about the most appropriate use of this treatment.
Talk with your doctor about which RSV prevention method is right for you and your child.
How Else Can I Protect Myself and Others From RSV?
Here are other steps to help protect yourself and others from RSV:
- Get the flu and COVID-19 vaccines to help avoid having more than one infection at the same time.
- If you have RSV or cold-like symptoms, stay home to reduce your chance of spreading it to other people.
- Wear a well-fitting face mask (N95) in crowded indoor spaces when respiratory infections are spreading, which is usually during the fall and winter.
- Cover your coughs and sneezes with a tissue or your upper shirt sleeve, not your hands.
- Wash your hands often with soap and water for at least 20 seconds.
- Avoid close contact, such as kissing, drinking after someone, shaking hands, and sharing utensils with others who are sick.
- Clean frequently touched surfaces, such as toys, doorknobs, and cell phones, often.
Parents and caregivers can protect children from getting RSV by following these steps:
- Get your child the flu vaccine if they are 6 months or older to reduce the chance that they will get the flu and RSV at the same time or reduce their risk of severe illness.
- Get your child the COVID-19 shot if they are 6 months or older to reduce the chance they will get COVID-19 and RSV at the same time or to reduce their risk of severe illness.
- Avoid close contact with sick people and stay home when you are sick.
- Wash hands often with soap and water for at least 20 seconds.
- Avoid touching faces, especially eyes, nose, and mouth, with unwashed hands.
- Talk with your child’s care center or school about what steps they take to reduce RSV spread.
- Have a backup child care plan in case it is needed.
- When possible, limit the time you spend in highly contagious settings during RSV season (usually September through January).
Medical Review: October 2024 by John James, MD
Closed Accordion
References
- About RSV. (2024, August 30). Centers for Disease Control and Prevention. https://www.cdc.gov/rsv/about/index.html
- Respiratory Syncytial Virus (RSV). (2024, June). National Foundation for Infectious Diseases. https://www.nfid.org/infectious-disease/rsv/
- RSV in Infants and Young Children. (2024, August 30). Centers for Disease Control and Prevention. https://www.cdc.gov/rsv/infants-young-children/









