Asthma
Pneumonia
Pneumonia is an infection of the lungs usually caused by viruses or bacteria. It can sometimes feel like a bad cold or the flu. It can also lead to serious, life-threatening illness and, in some cases, death.
Anyone can get pneumonia, but people with asthma are at higher risk for getting it. If you have asthma, you should know how to protect yourself from developing pneumonia.
What Is Pneumonia?
Your lungs have tiny air sacs that fill with air when you breathe in, bringing oxygen into your bloodstream and filtering out carbon dioxide when you breathe out. When you have pneumonia, these air sacs, called alveoli, can become inflamed and filled with fluid. It becomes hard for the oxygen you breathe in to reach your bloodstream, making it hard or even painful to breathe. Because the alveoli are filled with fluid, you may begin to have a cough that produces mucus and other symptoms.
There are many factors that can affect how serious pneumonia can be for you, such as:
- Age (such as very young children and older adults)
- General overall health
- Co-existing health conditions (such as asthma and other chronic lung diseases)
- The type of germ (such as a virus, bacteria, or fungi) that is causing your pneumonia
People at risk of pneumonia include:
- Children younger than 2 years old
- Adults with weakened immune systems or chronic health conditions (such as asthma, chronic obstructive pulmonary disease, or heart disease)
- Adults 65 and older
Pneumonia can be serious. About 1.4 million Americans go to the emergency department each year for pneumonia.1 Around 41,000 Americans die each year from pneumonia.1
What Are the Symptoms of Pneumonia?
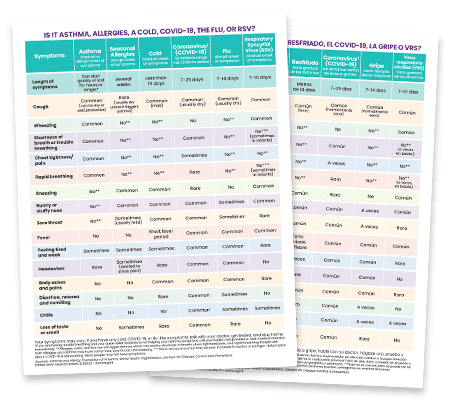
While every person may have different symptoms of pneumonia, there are some common symptoms with this disease. They can vary from mild to severe. The symptoms can usually appear suddenly or gradually over time. Many symptoms are similar to symptoms of the flu, but last longer. You may have some of the following symptoms if you get pneumonia:
- Trouble breathing (such as shortness of breath or rapid breathing)
- Chest pain (a sharp or stabbing pain when you breath in)
- Cough (you may cough up greenish or yellow mucus)
- Fever
- Sweating and chills
- Stiff neck
- Fatigue, tiredness, restlessness, weakness, or fussiness (in babies and young children)
- Loss of appetite
- Nausea, vomiting, or diarrhea
Call your doctor right away if you have a fever of 102 F or more or a persistent cough.
What Are Emergency Signs and Symptoms of Pneumonia?
Pneumonia can be serious and life-threatening. Call 911 if you or your child has any of these emergency symptoms:
- Rapid breathing or trouble breathing
- Severe chest pain
- Severe dizziness
- Severe headache
- A very high fever
- Cyanosis – tissue color changes on mucus membranes (like tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
- Serious or constant vomiting
- Sudden change in mental state, confusion, or can’t think clearly
- Not waking up, not interacting, or not conscious
Are People with Asthma at Risk for Pneumonia?
For people with asthma, pneumonia can be very serious. But doctors don’t fully understand why. It may be because airways with asthma are different because of chronic inflammation, swelling, and over-reactivity. Asthma may make the lungs more likely to be affected by infection. Corticosteroids, a common asthma medicine, may also increase your risk because they can suppress your immune system.2,3,4
What Causes Pneumonia?
Pneumonia infections can be caused by different organisms like bacteria, fungi, and viruses. Some common viruses that can cause pneumonia are:
- Flu (influenza) viruses
- Respiratory syncytial virus (RSV)
- Coronaviruses including COVID-19 (SARS-CoV-2 virus)
- Common cold (rhinovirus)
- Human metapneumovirus (HMPV)
- Human parainfluenza virus (HPIV)
- Adenovirus
Common bacteria that can cause pneumonia:
- Streptococcus pneumoniae (causes pneumococcal disease)
- Mycoplasma pneumoniae1
- Legionella pneumophila, which causes Legionnaires’ disease
- Chlymdia pneumoniae
- Haemophilus influenza type b (Hib)
Less often, illnesses like whooping cough, measles, and chickenpox can cause pneumonia. Vaccines are available for these illnesses. Getting these vaccines – along with the flu, COVID-19, RSV (if you are eligible), and pneumococcal vaccines – can help reduce your chances of getting pneumonia.
What Are the Different Types of Pneumonia?
There are different types of pneumonia based on what caused the pneumonia and where you caught it.
1. Community-acquired pneumonia: This is when someone gets pneumonia from their community or surroundings (not in a hospital). This is the most common type of pneumonia. It can be caused by:
- Bacteria: The most common cause of bacterial pneumonia in the U.S. is Streptococcus pneumoniae. You can inhale it into your lungs, or it can travel through your bloodstream to your lungs. It happens most often after you have had a cold or the flu. It may affect only one lung.
- Fungi: If you have a weakened immune system or chronic health problems, you are at higher risk for this type of pneumonia. It is caused by fungi (living organisms such as yeasts, molds, and mushrooms) that are inhaled or found in soil or bird droppings.
- Viruses: This is the most common cause of pneumonia in children under age 5. Viral pneumonia is usually mild, but it can sometimes be serious. Some of the viruses that cause the common cold and flu can cause this type of pneumonia. The COVID-19 virus can cause pneumonia, which can become severe. See above for a full listing of viruses that can cause pneumonia.
2. Health-care-associated pneumonia: This is when someone gets pneumonia during or following a stay in a hospital, health care setting, a nursing home, or a rehab center. Also, you can also get this type of pneumonia from outpatient centers, like dialysis centers. This type of pneumonia is typically caused by bacteria that may be more resistant to antibiotics. It can be serious and life-threatening because the people who get it are already sick.
3. Ventilator-associated pneumonia: This happens when you get pneumonia after being on a ventilator (a machine that helps you breathe or breathes for you by blowing air into your lungs). People who are at risk for this type of pneumonia are typically on a ventilator (a breathing machine) in an intensive care unit (ICU) in a hospital.
What Do People with Asthma Need to Know About Pneumococcal Disease?
Pneumococcal [noo-muh-kok-uhl] disease is a type of pneumonia caused by the bacteria Streptococcus pneumoniae or pneumococcus. This type of bacteria can cause many types of infections in your body, such as:
- Lung infections
- Blood infections
- Sinus infections
- Ear infections
- Meningitis (a serious infection of the lining of the brain and spinal cord)
Some of these infections can be life-threatening and may require a stay in the hospital.
Anyone can get pneumococcal disease, but some people are more at risk than others. People at higher risk of getting pneumococcal disease include:
- Children younger than 2 years old
- Adults 65 and older
- People with chronic health conditions or weakened immune systems
If you have had a pneumococcal infection in the past, it will not keep you from getting it again.
Vaccines are the best way to prevent pneumococcal disease. There are 2 kinds of vaccines to prevent pneumococcal disease:
- Pneumococcal conjugate vaccines (PCVs)
- Pneumococcal polysaccharide vaccine (PPSV)
These vaccines protect against many but not all types of pneumococcal bacteria. The Centers for Disease Control and Prevention (CDC) recommends different PCVs for different people based on age and medical status. Talk with your doctor about your options.
In 2024, a pneumococcal conjugate vaccine (PCV21) became an option for adults 19 and older. This vaccine can help protect against new strains in pneumococcal disease, which are on the rise. The CDC recommends all adults aged 50 and over get routine adult pneumococcal vaccination. Adults who are 19-49 years old with a risk condition such as chronic lung disease or immunocompromising conditions should also get the pneumococcal vaccine.6 (See the list of risk conditions on the CDC website.)
Specific pneumococcal vaccines have been recommended for all U.S. infants and young children since 2000. These vaccines have worked well protecting infants from the infection.6 Talk with your doctor about which pneumococcal vaccine is most appropriate for your infant or young child.
It is also important to get the flu vaccine every year. Getting the flu increases your chances of getting pneumococcal disease.
How Does Pneumonia Spread?
You can spread pneumonia in several ways. You can spread it through coughing, sneezing, or direct contact (like kissing). You can even spread it through contact with blood. Not everyone who carries the bacteria or virus gets sick from it. That means it is possible to catch it from someone who seems to be healthy.
How Do Doctors Treat Pneumonia?
If you have pneumonia, treatment will depend on what type you have and how sick you are. Bacterial pneumonia can be treated with antibiotics and other supportive medical measures, such hydration and supplemental oxygen, if needed.
If your pneumonia is related to the flu or COVID-19, you may be given antiviral medicines and antibiotics, if needed. If you have a weakened immune system, you may be treated for a fungal infection.
Your doctor may also give you a corticosteroid, if needed. If your pneumonia is severe, you may require a hospital stay for more intensive medical treatment and observation.
If you get pneumonia, be sure to rest and drink plenty of liquids to help you recover. If your symptoms don’t get better, call your doctor right away.
It can take weeks or months to fully recover from pneumonia.
How Can I Protect Myself from Pneumonia?
The best way you can avoid getting pneumonia is to get a vaccine. Getting the vaccines for pneumococcal disease, Haemophilus influenzae type b (Hib), COVID-19, the flu, whooping cough (pertussis), RSV (if you are eligible), and measles is the most effective way to prevent pneumonia. Medicare and most insurance companies will pay for these vaccines. Talk with your doctor about specific risks and benefits of these vaccines.
Many people get the pneumococcal vaccine when they are children. But you may need another shot when you are an adult. Talk with your doctor to find out if you need another pneumococcal shot.
Practicing good hygiene can also help keep you healthy and from getting and spreading pneumonia. You can prevent infections by:
- Washing your hands with warm soapy water for 20 seconds or longer (or using an alcohol-based hand sanitizer if soap and water are not available)
- Cleaning and disinfecting community surfaces
- Coughing or sneezing into a tissue
- Limiting contact with tobacco or e-cigarette smoke or quitting smoking
- Wearing a mask in public indoor spaces when respiratory infections are spreading in your community
- Keeping your asthma under control
Do the Flu and COVID-19 Vaccines Protect Me from Pneumonia?
The flu (influenza) and COVID-19 can affect your respiratory tract (lungs, nose, throat) and cause swelling and inflammation of the airways. This can increase your risk of pneumonia.
The best way to protect yourself from the flu is to get the vaccine every year between September and October. Get your shot at the beginning of flu season, which usually starts in October and ends in May. If you miss getting the flu vaccine in early fall, you can get it any time during the flu season. It takes about 2 weeks for your body to start building immunity after receiving the flu vaccine.
Also, it is important to stay up to date with COVID-19 vaccines. The COVID-19 vaccine can help prevent serious symptoms (including pneumonia) if you get sick with COVID-19.
You can get the flu shot and COVID-19 shot at the same time.
Medical Review: February 2025 by John James, MD
Closed
References
- FastStats – Pneumonia. (2019). Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/fastats/pneumonia.htm
- Centers for Disease Control and Prevention (CDC); Advisory Committee on Immunization Practices. Updated Recommendations for Prevention of Invasive Pneumococcal Disease Among Adults Using the 23-Valent Pneumococcal Polysaccharide Vaccine (PPSV23). MMWR Morb Mortal Wkly 2010 Sep 3;59(34):1102-6. PMID: 20814406.
- Lee TA, Weaver FM, Weiss KB. Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med 2007 Jan; 22(1):62-7.
- Talbot TR, Hartert TV, Mitchel E, Halasa NB, Arbogast PG, Poehling KA, et al. Asthma as a risk factor for invasive pneumococcal disease. New England Journal of Medicine 2005; 352(20):2082-90.
- Aliberti, S., Dela Cruz, C. S., Amati, F., Sotgiu, G., & Restrepo, M. I. (2021). Community-acquired pneumonia. The Lancet, 398(10303), 906–919. https://doi.org/10.1016/s0140-6736(21)00630-9
- Centers for Disease and Control (CDC); (2024, October). CDC Updates Vaccine Recommendations. https://www.cdc.gov/ncird/whats-new/cdc-updates-vaccine-recommendations.html