Asthma
Managing Asthma and Respiratory Infections in Schools
Schools can face special challenges when respiratory infections are spreading. Common respiratory viruses include COVID-19, the flu, and RSV. These illnesses can impact both students and school staff who have asthma.
Respiratory Infections and Asthma
Asthma is one of the most common diseases in children. It is also one of the top causes of missed school days (otherwise known as absenteeism).1
Respiratory infections often spread the most in the fall and winter when children are in school. Schools have a large number of people inside together, and this can make illnesses spread easily and quickly.
Respiratory infections are caused by viruses or bacteria that make you sick. These infections affect the lungs, nose, sinuses, and throat, especially in people with asthma. They can affect other parts of the body too. They are a common asthma trigger, especially in children.
Some of the most common respiratory illnesses are:
- Colds (caused by many different viruses)
- COVID-19 (caused by the SARS-CoV-2 coronavirus)
- Flu (caused by the influenza virus)
- Respiratory syncytial [sin-SISH-uhl] virus (known as RSV)
- Pneumonia (caused by bacteria, virus, or fungus)
- Bronchitis (can be caused by a bacteria, virus, airway irritants, or other factors)
What Are the Symptoms of Respiratory Infections?
Many respiratory infections can cause a runny nose, fever, or sore throat. They can also cause symptoms like coughing and shortness of breath, which overlap with common symptoms seen with asthma. They may also cause sneezing, which is a symptom of seasonal allergies. Respiratory infections can also make asthma worse.
The Asthma and Allergy Foundation of America (AAFA) created a respiratory illness symptom chart to help you learn how to tell the difference between asthma, seasonal allergies, colds, COVID-19, flu, and RSV. It covers the differences in length of the illness and types of symptoms.
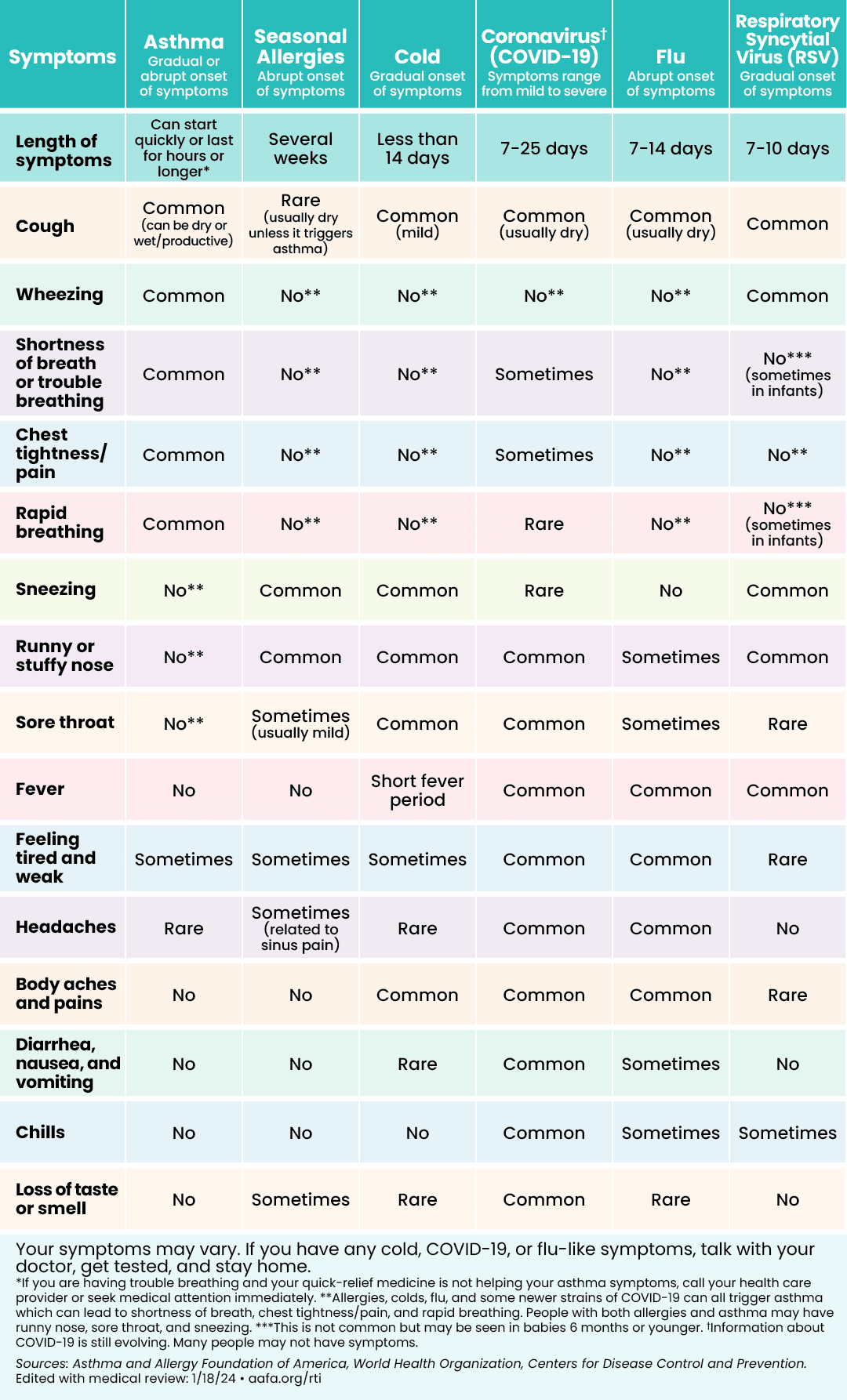 | 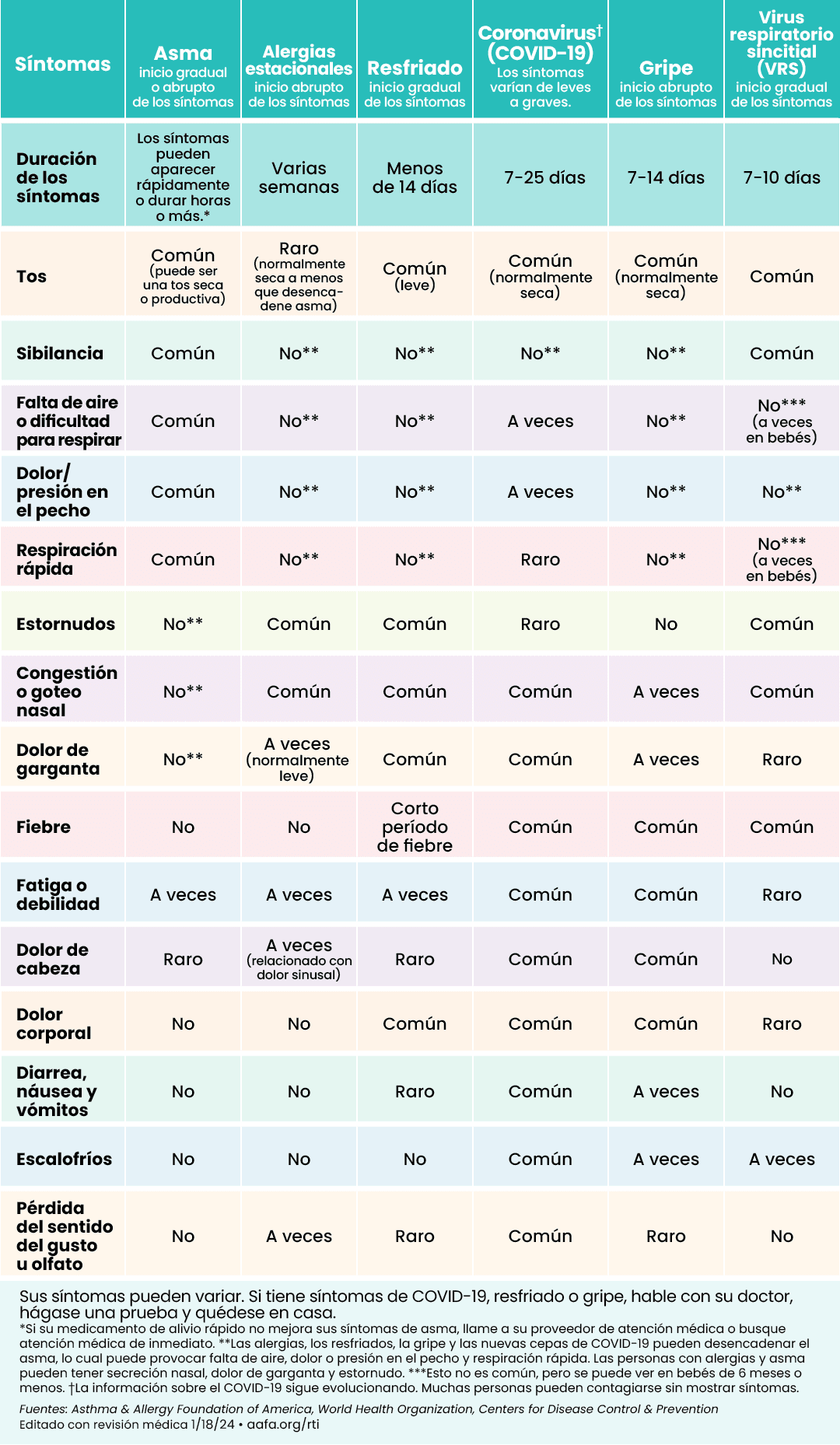 |
Click to see larger image (English) | Click to see larger image (Spanish) |
How Can Parents and Guardians Prevent Respiratory Illnesses?
Here are a few ways parents, guardians, and caregivers can reduce the spread of illness among school age children:
- Keep children home when they are sick. Respiratory infections can easily spread to other people. If your child is sick or has symptoms, keep them home, talk with your child’s doctor. Your child may need a test to diagnose their illness.
- Cover coughs and sneezes. If your child is sick, protect other people by having them wear a mask. Teach them to cover their coughs and sneezes with tissue or by coughing into their elbow if they do not have a mask on.
- Teach good handwashing. When someone who is sick coughs or sneezes into their hands, they can spread viruses to the next item or person they touch. Teach kids to wash their hands often with soap and warm water for at least 20 seconds to prevent spreading illnesses. Use an alcohol-based hand sanitizer if soap and water are not available.
- Stay up to date and vaccinate. Get the flu and COVID-19 vaccines every year according to recommended guidelines. These vaccines are authorized for children aged 6 months and older. These vaccines help protect your child from severe illness, emergency department visits, hospital stays, and death.

How Can Schools Prevent the Spread of Respiratory Illnesses?
Here are a few ways school policies, school staff, and volunteers can reduce the spread of illness in and around school:
- Support children (and staff) staying home when they are sick. Enact policies that allow children to stay home when they are sick. Students returning to school after a respiratory infection may still be contagious. Additional prevention strategies their family may choose include wearing masks, physical distancing, and testing (e.g. rapid detection testing for flu, COVID-19, RSV). Ask your doctor when it would be appropriate and how to perform this testing.
- Have staff wear masks when sick or when they have been exposed to a highly contagious illness. Masks can reduce the spread of viruses from person to person. When respiratory infections are spiking in your community, have staff wear masks if they are sick or have been exposed to someone who is sick. School staff providing care for a sick student should wear personal protective equipment (e.g. N-95 mask).
- Improve air filtration and ventilation. Opening windows/doors, changing air filters, doing regular maintenance on heating and cooling systems, and using Certified Asthma & Allergy Friendly® air cleaners can help improve airflow and the quality of indoor air in classrooms. This will help reduce virus particles in your indoor air. Additional steps for cleaner air in schools: Everyday Actions for Schools to Prevent and Control the Spread of Infections (CDC)
- Monitor air quality around campus. Use air quality monitors indoors and outdoors around school campus.
- Ask parents/guardians of students with asthma to provide inhalers instead of nebulizers, if possible. Nebulizers can spread virus particles through the air. A child may be infected with a virus before they show symptoms. Studies show that inhalers (used with a spacer if it is a metered dose inhaler) can work just as well as a nebulizer. If a child needs to use a nebulizer, have them use it in a separate room without other students present. Provide school staff administering nebulizer treatments with N-95 masks. Here is a sample letter to request inhalers instead of nebulizers.
- Stay up to date and vaccinate. Teachers, school staff, school volunteers, children, and their families can help keep the community healthy by staying up to date with all recommended vaccinations like the flu and COVID-19 vaccine.
The Centers for Disease Control and Prevention (CDC) also has information on what schools can do to plan for and prevent the spread of infections.
September Asthma Peak
September is often the worst month for people with asthma, especially children. During this month, there is an increase in asthma attacks, emergency room visits, asthma-related hospital stays, and even deaths. It is called Asthma Peak Month, or the September Asthma Epidemic.
Several factors can affect people with asthma at the same time during September. This is a common time for respiratory viruses to spread. Children return to school in the fall and are exposed to respiratory illnesses, such as the flu, RSV, COVID-19, and colds. Ragweed pollen, the most common fall pollen allergen, peaks in September in the United States. In addition, mold counts can go up as leaves collect outside. Finally, extreme weather events and wildfires can also expose people to asthma and allergy triggers as well.
Many school buildings and facilities throughout the U.S. have poor indoor air quality and they need ongoing maintenance and repair. This can expose children with asthma to allergens such as indoor mold, animal dander, dust, and pests, irritants, and other asthma triggers. Also, schools may use harsh, strong-smelling cleaning products or chemicals, which can trigger asthma.
Everyone with asthma needs to take extra precautions during September.
- Follow your Asthma Action Plan, which is developed with the help from your doctor. If your child has asthma, make sure their child care center, other caregivers, or school has a copy of this document on file.
- Talk with your doctor if your asthma is not well-controlled. They can make changes to your Asthma Action Plan if needed.
- Always carry your quick-relief medicines with you.
- Make sure you have all your necessary asthma medications, and they are not expired. In addition, make sure you have refills available.
- Get vaccines for the flu and COVID-19.
- Take steps to avoid getting sick, such as washing your hands, wearing a well-fitted N95 face mask, not touching your face, and avoiding people who are sick.
- Avoid your asthma and allergy triggers as much as possible.
How Does Indoor Air Quality Affect Students and Staff with Asthma?
Students are healthier and learn better when their indoor air is cleaner. When children don’t have asthma symptoms triggered by poor air quality, they are more likely to do better in school.
Asthma triggers – including allergens, chemicals, and volatile organic compounds (VOCs) – are common in many school buildings and create poor indoor air quality (IAQ). Reducing these potential triggers is a key part of asthma control.
When illnesses are spreading, schools may clean more often with harsh chemicals. This can have a negative impact on air quality. They can be an asthma trigger and can irritate the airways of students and staff with asthma.
Unhealthy IAQ can lead to more asthma symptoms. This can then lead to more missed school days, emergency room visits, and even hospital stays. Children with uncontrolled asthma may struggle to learn and could fall behind in their schoolwork.
Schools can make changes to improve IAQ. Improving IAQ not only creates a healthier school but promotes better learning as well. Many of these changes can be simple. Here are some ways schools can improve IAQ:
- Clean with non-scented and less harsh chemicals.
- Use only district-approved and provided cleaning products.
- Don’t allow children to clean any hard surfaces in the school.
- Use integrated pest management.
- Don’t keep furry pets in the classroom to reduce pet dander.
- Fix leaks quickly to reduce the chance of mold.
- Place Certified Asthma & Allergy Friendly® air cleaners in classrooms with children or teachers with asthma if the room has poor ventilation.
If you do run air cleaners in school rooms, make sure they do not have an ionizer (ozone) function. Or if they do, make sure you can turn the function off. Ionizers and ozone can trigger asthma symptoms. They have not been proven to remove the virus that causes COVID-19 from the air.2
Medical Review: October 2024 by John James, MD
Closed
References
- Nurmagambetov, T., Kuwahara, R., & Garbe, P. (2018). The Economic Burden of Asthma in the United States, 2008–2013. Annals of the American Thoracic Society, 15(3), 348–356. https://doi.org/10.1513/annalsats.201703-259oc
- Will an Ozone Generator protect me and my family from COVID-19? (2024, August 27). Retrieved October 18, 2024, from https://www.epa.gov/indoor-air-quality-iaq/will-ozone-generator-protect-me-and-my-family-covid-19
Managing Asthma and Allergies at School
- School Health Care Plans for Asthma and Allergies
- 504 Plans for Asthma
- School Forms for Asthma
- School Planning Resources for Parents of Children with Asthma & Allergies
- Resources for Schools and Care Centers
- Resources for Early Childhood Education and Child Care
- Managing Asthma and Respiratory Infections in Schools










