Allergies
Cockroach Allergy
What Is Cockroach Allergy?
There are 25 species of cockroaches. Cockroaches contain different proteins that may be allergens for many people. An allergen is a substance that causes an allergic immune reaction. The body parts, saliva, feces, and waste of cockroaches are allergens. Even dead cockroaches can cause allergic reactions.2
When kicked up in the air, cockroach particles may become airborne, get into the nose and/or mouth, and get breathed into the lungs, causing an allergic response and triggering nasal (nose) symptoms or asthma attacks.2,3
What Are the Symptoms of Cockroach Allergy?
Common cockroach allergy symptoms include:3,4
- Sneezing
- Runny nose
- Itchy, red, or watery eyes
- Stuffy nose
- Itchy nose, mouth, or throat
- Postnasal drip (a flow of mucus from behind your nose into your throat)
- Cough
- Itchy skin or skin rash
- Ear infection
- Sinus infection
If your cockroach allergy triggers your asthma, you may also have:4
How Do Doctors Diagnose Cockroach Allergy?
To diagnose a cockroach allergy, your doctor will start with taking your medical history for symptoms and perform a physical exam. If your doctor thinks you may or could have a cockroach allergy, he or she may suggest a skin prick test or a specific IgE blood test.
People who live in certain areas and have symptoms year round are often found to have a cockroach allergy, among other possible indoor allergies.2,3
Skin Prick Test (SPT)
In prick/scratch testing, a small drop of the allergen in question is pricked or scratched on your skin. If you are allergic to the substance, you will develop redness, swelling, and itching at the test site within 20 minutes. You may also see a wheal, which is a raised, round area that looks like a hive. Wheals will itch temporarily. Usually, the larger the wheal, the more the body recognizes the allergen, though this does not always mean it causes more symptoms than something with a smaller wheal.
A positive SPT to a particular allergen alone does not necessarily mean you have an allergy. Your allergy specialist must compare the skin test results with your history, to see if the symptoms match the testing. Skin testing is done in the office and results take 15-20 minutes.
Specific IgE Blood Test
Blood tests are another way to test for allergies. These detect antibody in the blood, whereas the skin test detects local antibody already on the cell that causes an allergic reaction. Both tests tell if you make antibody to an allergen.
Blood tests can be helpful when people have a skin condition or are taking medicines that interfere with skin testing. They may also be used in children who may not tolerate skin testing.
Both blood testing and skin testing can test multiple allergens at the same time. Your doctor (or the office lab) will take a blood sample and send it to be analyzed, where allergen is added to your blood sample. This measures the amount of antibodies your blood produces, along a scale of 0.1 kilounits of antibody to >100 kilounits of antibody.
Reporting is also done in one of 6 classes, depending on how much antibody is detected. This test is called Specific IgE (sIgE) Blood Testing (most commonly as ImmunoCAP testing). As with skin testing, a positive blood test to an allergen does not necessarily mean that an allergen caused your symptoms, and your doctor has to assess this.
What Is the Treatment for Cockroach Allergy?
The most important step is to avoid cockroaches as much as possible. Limiting your exposure to cockroaches will reduce your symptoms. However, you may also need medicines to control allergy symptoms.3,4
Certain over-the-counter (OTC) and prescription medicines, such as antihistamines and corticosteroid [kor-tick-OH-stair-ROID] nasal sprays, may help reduce allergy symptoms. Talk to your doctor about what medications may be right for you.4 These medications treat any allergy symptoms, not just those caused by cockroach.
Allergy Medicine Guide
Nasal rinse: Using a saline (saltwater) nose rinse can help cut down mucus and rinse allergens out of your nose. Remember to use these as directed. This does not protect against the allergen but can help with nasal symptoms.
Corticosteroid nasal sprays reduce inflammation (swelling) in the nose and block allergic reactions from developing. They are the most effective medicine type for allergic rhinitis because they can reduce all symptoms, including nasal congestion. They can also provide some relief for eye allergy symptoms. Nasal corticosteroids have few side effects (e.g., headache, nose bleeds or irritation). Many are now available over-the-counter without prescription.
Corticosteroid nasal sprays: FLONASE®, Nasacort®, Nasonex™, Nasalide/Flunisolide, Omnaris™, QNASL®, RHINOCORT®
Antihistamines relieve sneezing and itching in the nose and eyes. They also reduce a runny nose and, to a lesser extent, nasal stuffiness. Look for a long-acting, non-drowsy antihistamine. The newer forms do not carry the risk of toxicity (like feeling drowsy) that has been associated with older antihistamines like diphenhydramine. Certain antihistamines may come as nasal sprays.
Non-steroidal antihistamine nasal sprays (may cause drowsiness): Astelin®, Astepro®, Patanase®
Non-drowsy oral antihistamines: Allegra®, CLARINEX®, Claritin®
Oral antihistamines that may cause drowsiness in some individuals: Xyzal®, ZYRTEC®
Cetirizine (ZYRTEC®) and loratadine (Claritin®) are the antihistamines of choice for use during pregnancy. They have established safety profiles and are effective in treating allergy symptoms during pregnancy.
Diphenhydramine and related short-acting antihistamines (like promethazine) should be avoided. Diphenhydramine (known under the brand name BENADRYL®) is not a good choice to take for allergy symptoms because of its short-term action to manage symptoms and several known negative side effects. The major side effects of diphenhydramine and older generation antihistamines include drowsiness, sedation, dry mouth/eyes, and fatigue. This can also impair alertness, concentration, multitasking, and memory. In turn, this antihistamine can affect important functions, such as learning and test performance in children, as well as operation of machinery and cars in adults. As these medicines can impair you, they can affect work performance and safety. Side effects may worsen with higher dosing that is used for other conditions such as chronic hives.
Eye drops: Allergy eye drops can relieve eye burning, itchiness, redness, increased tearing, and swelling. These can come in a few types - antihistamine, mast cell stabilizers, and steroid eye drops. Many antihistamine eye drops are sold over the counter.
Antihistamine eye drops: Azelastine/Optivar, Bepreve®, Elestat®, LASTACAFT®, Opcon-A®, Systane® ZADITOR®, Patanol™, and Pataday®
Decongestants help shrink the lining of the nasal passages and relieve nasal stuffiness. They generally are only used for a short time (3 days). Read the instructions carefully and do not use them for extended amounts of time. Extended use of decongestant nasal sprays can cause a rebound effect that worsens your congestion. Make sure you talk with your doctor about the appropriate use of decongestants, limitations, and potential side effects.
Nasal spray decongestants: Afrin®, Vicks Sinex™
Oral decongestants: SUDAFED®
Some allergy medicines combine an antihistamine with a decongestant. Certain types of combo medicines (such as the ones that contain pseudoephedrine as the decongestant) are available “behind the counter”. Behind-the-counter products are available without a prescription but have limitations on purchases due to state and federal laws. Talking with pharmacy staff is generally necessary to obtain these types of allergy medications.
Decongestant + antihistamine combos: Allegra-D®, Claritin-D®, Clarinex-D, ZYRTEC-D®
Check with your doctor before using decongestants if you have high blood pressure, heart disease, glaucoma, thyroid disease, or trouble urinating. They may cause issues if you have any of these conditions and they may interact with other prescription medicines.
Federal Regulations on Decongestants
The oral form of phenylephrine (PE) is a common active ingredient in many OTC decongestants. An expert panel of the FDA reviewed studies which showed oral PE is not effective at relieving nasal congestion in commonly used doses. The FDA is proposing to end use of oral PE. This would remove these products from the U.S. market. The change would not affect the nasal spray forms of PE.
Decongestants that contain pseudoephedrine (PSE) require photo identification and are only available to purchase behind the pharmacy counter.
Cromolyn sodium is a nasal spray that blocks your body from releasing chemicals (such as histamine and leukotrienes) that cause allergy symptoms including histamine and leukotrienes. This medicine has few side effects, but you must take it three to six times a day. For optimal results, this medication should be used daily during your allergy season. It can be started up to one week before your allergy season begins.
Cromolyn sodium nasal spray: NasalCrom®
Leukotriene receptor antagonists (or modifiers) block the action of important chemical messengers (other than histamine) that are involved in allergic reactions. These medicines help manage asthma and allergic rhinitis symptoms. These medications are taken orally. How often you take them depends on the specific drug. Discuss the appropriate use of these medications with your doctor, including the risks and benefits of therapy.
Options include: ACCOLATE®, SINGULAIR®*, Zyflo CR®
*Note: Montelukast (brand name SINGULAIR®) has a black box warning because it can cause serious mental health side effects. This is a safety warning from the Food and Drug Administration (FDA). This means you need to be aware of a drug’s side effects or important instructions for safe use of the drug. We encourage you to speak with your health care provider before, during, and after the start of any new medicine. If your doctor recommends montelukast, talk with them about possible risks and concerns.
Medical Review: March 2025 by John James, MD
Some people with a cockroach allergy do not get complete relief from the combination of cockroach avoidance actions and medicines. In some cases, your allergist may then consider immunotherapy [eh-mu-no-THER-ah-pee] (allergy shots).2
Immunotherapy is a long-term treatment (3-5 years) that can help prevent or reduce the severity of allergic reactions and sometimes decrease risk of asthma triggered by allergens. It can change the course of allergic disease by reducing the body’s immune response to allergens. While many people choose to try medicines first, allergy shots are also a possible first strategy.
There are two types of immunotherapy: allergy shots and sublingual immunotherapy.
Allergy Shots – subcutaneous immunotherapy (SCIT) has been around for more than 100 years and can provide long-lasting symptom relief. SCIT is a series of shots that have larger amounts of allergen in each shot. The allergen will be injected into the fat under the skin. Over time, allergic symptoms generally improve. Many people get complete relief within one to three years of starting SCIT. Many people also feel the benefits for at least several years after the shots stop.
Sublingual (under-the-tongue) immunotherapy (SLIT) involves placing a tablet with the allergen under your tongue for one to two minutes and then swallowing it. This treatment offers people with these allergies a potential alternative to allergy shots.
Your doctor may also do SLIT using drops of cockroach extract. Global data show this is safe and effective but has not been studied in the U.S. to be approved by the Food and Drug Administration (FDA) at this time.
Talk with your allergist about your allergy symptoms and your allergy treatment plan.
How Can I Prevent Allergic Reactions to Cockroaches?
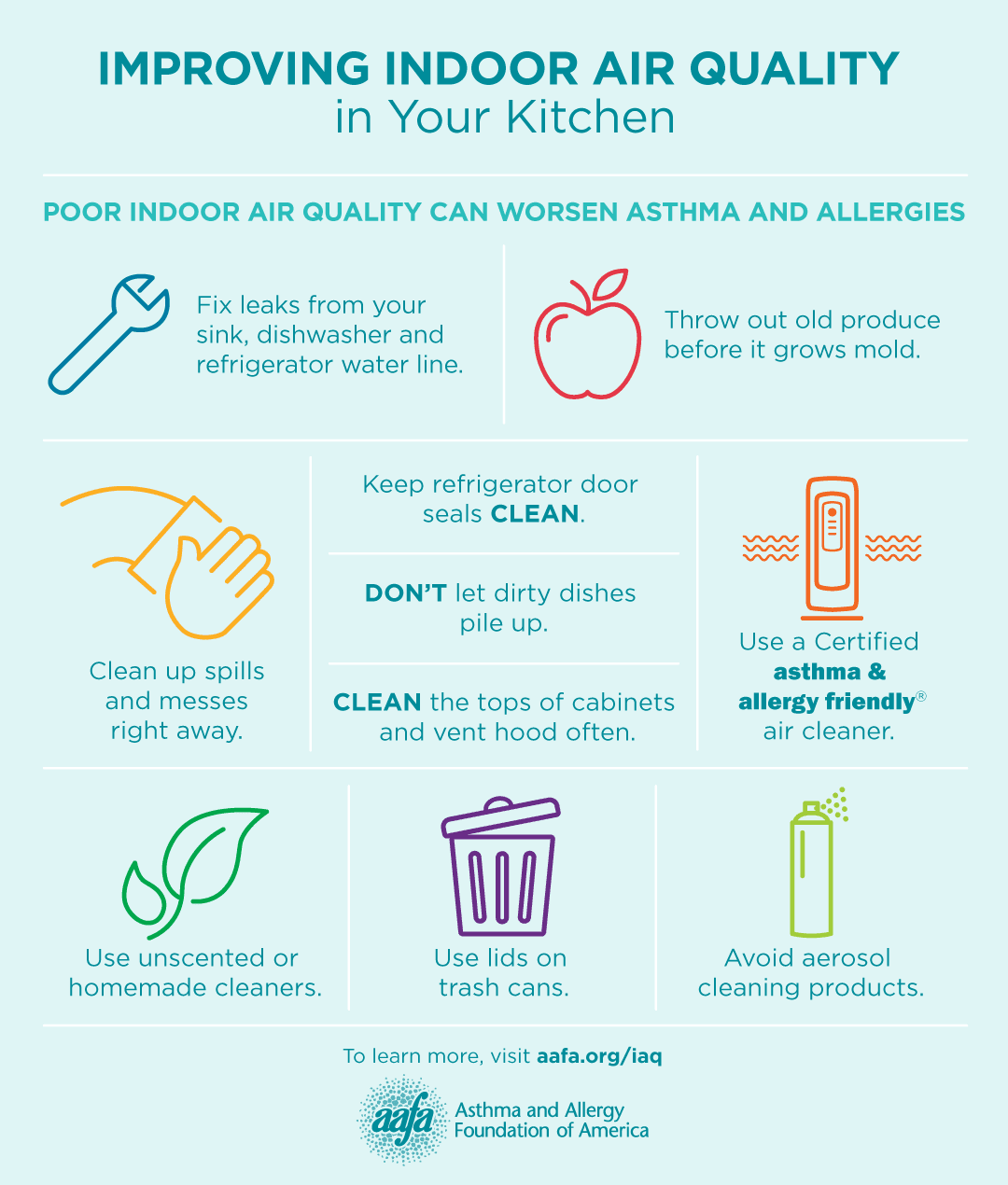
Avoid exposure to cockroaches and their droppings. This may be hard to do, because cockroaches are in most environments, especially in inner cities. Pests need food, water and shelter to survive. There are changes you can make to your home to reduce the numbers of these unwanted “guests”:3,4
- Cover all trash cans tightly.
- Store food in airtight containers. This includes food kept in cabinets and on counters.
- Clean all dirty dishes. Do not leave them in the sink or on the counter.
- Sweep up any food crumbs from the counters, stove top, tables, and floor. Wipe up any spills. Vacuum and mop floors regularly.
- Avoid leaving pet food out in a bowl. Clean the bowl regularly, like other dirty dishes.
- Fix leaky pipes under sinks and in the basement. Cockroaches like damp places.
- Seal cracks in the walls and floors where cockroaches can enter your home.
- Avoid piles. This includes piles of magazines, laundry, or newspapers, as cockroaches like to hide in dark, cluttered places such as these ones.
- Use cockroach baits and traps. These may be better choices than sprays. Sprays may irritate allergies and asthma in some people.
If you have a cockroach infestation in your home, you should consider contacting a pest control professional.
How Can I Identify Cockroaches?
Cockroaches have oval-shaped, flat bodies, with six long legs covered with spines, and range in color from black to reddish-brown. These insects have long antennae about the length of their body. Many adult cockroaches have wings, but only a few are capable of flying. Young cockroaches resemble adults but are smaller and do not have wings.
Cockroaches are active at night and hide during the day. These insects can be found worldwide and are one of the most common house pests. Cockroaches can multiply very quickly, and thrive in humid, warm, and dirty environments.5,6
Closed
References
- United States Environmental Protection Agency. (2025, March 13). Cockroaches and Schools. Retrieved May 23, 2025, from: https://www.epa.gov/ipm/cockroaches-and-schools
- Do, D.C., Zhao, Y., & Gao, P. (2016). Cockroach allergen exposure and risk of asthma. Allergy, 71(4), 463-74. https://doi.org/10.1111/all.12827.
- American College of Allergy, Asthma and Immunology. (2018, February 1). Cockroach Allergy. Retrieved May 23, 2025, from: https://acaai.org/allergies/allergic-conditions/cockroach-allergy.
- Cleveland Clinic. (2023, September 1). Cockroach Allergy. My Cleveland Clinic. Retrieved May 23, 2025, from: https://my.clevelandclinic.org/health/diseases/25229-cockroach-allergy.
- University of Minnesota. (2024). Cockroaches. University of Minnesota Extension. Retrieved May 23, 2025, from: https://extension.umn.edu/insects-infest-homes/cockroaches.
- Tang, Q., Vargo, E. L., Ahmad, I., Jiang, H., Varadínová, Z. K., Dovih, P., Kim, D., Bourguignon, T., Booth, W., Schal, C., Mukha, D. V., Rheindt, F. E., & Evans, T. A. (2024). Solving the 250-year-old mystery of the origin and global spread of the German cockroach, Blattella germanica. Proceedings of the National Academy of Sciences, 121(22):e2401185121. https://doi.org/10.1073/pnas.2401185121.